The study focused on 1,345,561 prostate cancer patients diagnosed between 2004 and 2015 using the national cancer database (NCDB). The rare variants included ductal, neuroendocrine (NEC), mucinous, signet ring cell (SRC), and adenosquamous prostate cancer. The descriptive characteristics of these patients were stratified by their histology and compared to nonvariant prostate cancer. Lastly, Cox regression analysis was performed to study the effect of histological subtype on overall mortality.
Less than 1% of the patients (0.38%) presented with rare-variant prostate cancer. All the rare variant patients presented with a higher clinical T stage when compared to the non-variant prostate cancer patients (p<0.001). The SRC, mucinous and ductal variants presented with a significantly higher biopsy grade (Gleason grade group >=4 – 34.7%, 11.2%, and 27% respectively, vs. 8.6% of the nonvariant patients, p<0.001). The key results are presented in figure 1 with the percentage of patients presenting with metastatic disease, the median PSA at presentation, the percentage of patients presenting with clinical stage >=T3, and the estimated overall survival of these patients. The Cox regression model, after adjusting for all relevant covariates, demonstrated that mortality was significantly higher in the ductal, SRC, adenosquamous, and NEC variants when compared to the nonvariant patients.
Figure 1 – Key results of analyses:
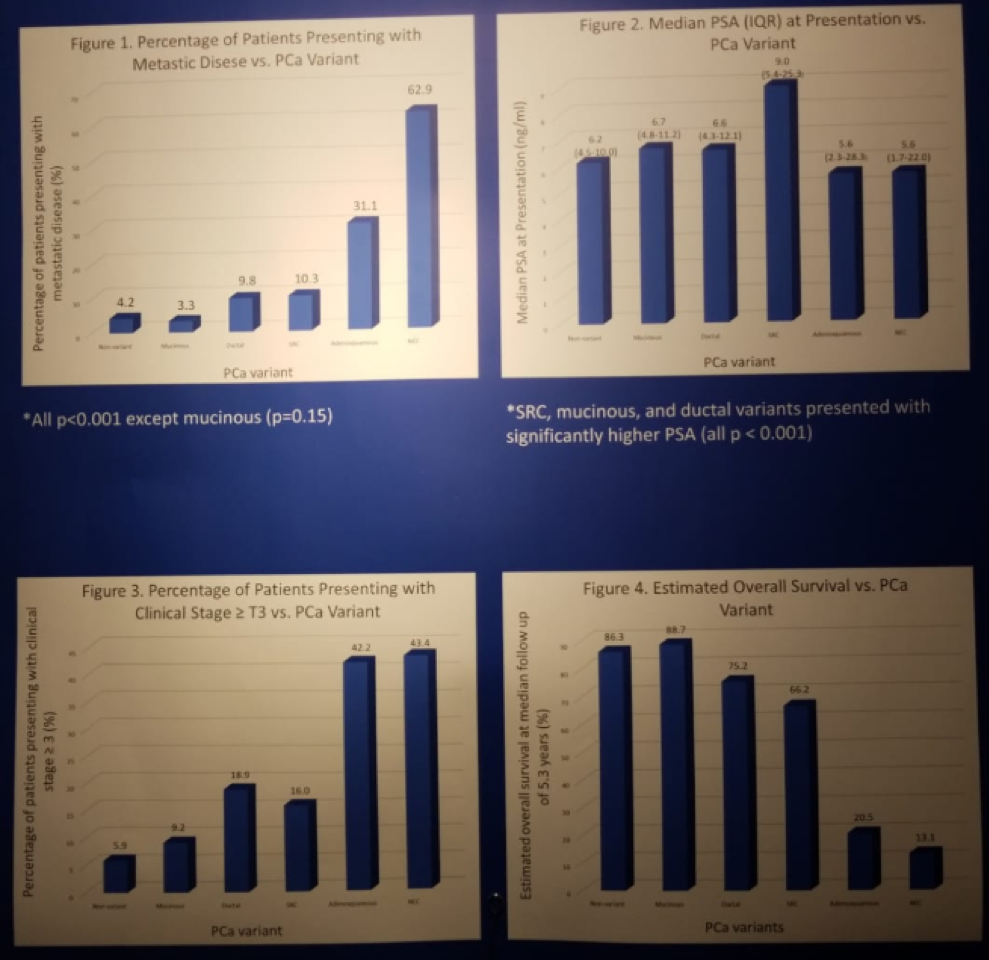
In conclusion, the authors noted that there are differences in the presentation and overall survival of rare prostate cancer variants when compared to the standard nonvariant cancer. Presentation with metastatic disease is more common among these rare variants, and all of them also presented with a higher local stage then the nonvariant patients. Lastly, NEC variant is associated with the worst, and the mucinous variant is associated with the best overall survival.
Despite this study using a very large database, the absolute number of these cases is relatively small, and more data needs to be collected on these cases in future studies.
Presented by: Sohrab Arora Vattikuti, Senior Fellow, Department of Urology, Urology Institute, Henry Ford Hospital, Detroit, Michigan, United States
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.


