Barcelona, Spain (UroToday.com) There are several preoperative risk stratification models in prostate cancer that assess the risk of recurrence following radical prostatectomy. However, not all patients who experience biochemical recurrence ultimately progress to clinical recurrence and die from their disease. The authors of this presented study aimed to develop and externally validate a novel risk classification tool predicting clinical recurrence at long-term follow-up in European patients that were treated with radical prostatectomy.
For the purpose of this study, 19,825 patients with prostate cancer who were treated with radical prostatectomy between 1991 and 2018 at two European tertiary referral centers were identified. The main outcome was 8-year clinical recurrence defined as positive imaging during follow-up after the onset of biochemical recurrence. The authors also performed multivariable cox regression model to predict clinical recurrence in patients treated at one institution (development cohort). This model represented the basis for a coefficient based nomogram which was later externally validated in the second institutional cohort. The covariates in the model included PSA at radical prostatectomy, biopsy Gleason grade group, clinical T stage, and percentage of positive cores at biopsy. The authors also performed Receiver operating characteristics (ROC) derived area under the curve (AUC) and decision curve analyses to compare the accuracy of the model to the D’Amico risk classification and CAPRA score in the prediction of 8-year clinical recurrence. Lastly, the authors developed a novel risk score using the nomogram-derived coefficients.
The data showed that the median age of the included patients at surgery was 63.7, with 72% of patients having a PSA<10, 20% having a PSA between 10-20, and 8% having a PSA >20. A total of 75% of the patients were clinical stage T1c, 23% were T2, and 2% were >=T3. Most patients had a biopsy Gleason grade group of 1 (43%), 28% had Gleason grade group 2, 13% had Gleason grade group 3, and 16% had Gleason grade group 4-5. Lastly, 44% of patients had <33% involvement of positive cores, 37% had 33-66% core involvement, and 19% had more than 66% core involvement.
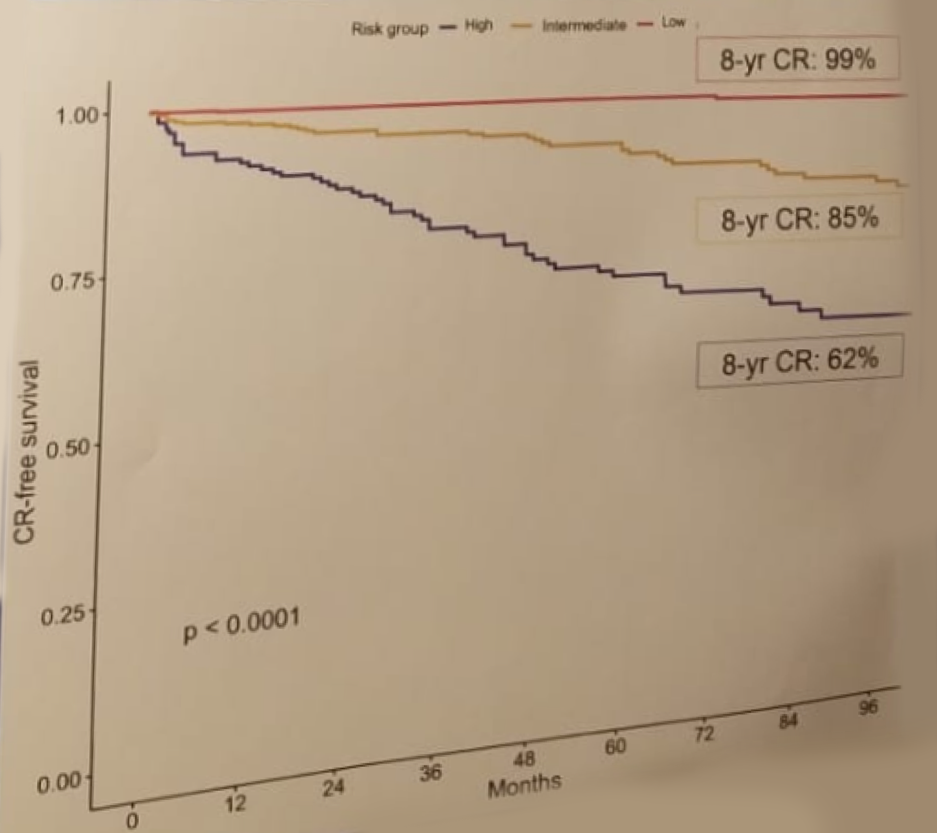
Table 1 demonstrates the results of the univariate and Cox regression multivariable model. This model showed that statistically significant predictors of clinical recurrence included clinical stage T2 and T3 compared to T1c, biopsy Gleason grade group 3,4 and 5 (compared to Gleason grade group 1), and >66% positive core involvement (compared to <33% core involvement). Figure 1 demonstrates the calibration plot and nomogram based on the Cox regression model predicting clinical recurrence at 8 years. Lastly, figure 2 shows the decision curve analysis comparing the accuracy of the novel risk tool presented in this study vs. the D’Amico risk classification and the CAPRA score. Table 2 shows the final developed nomogram-derived risk score, and figure 3 demonstrated the Kaplan-Meier plot depicting clinical recurrence-free survival stratified by the nomogram risk groups.
Table 1 – Univariate and Cox regression multivariable model predicting clinical recurrence:
Figure 1 – Calibration plot and nomogram based on Cox regression model predicting clinical recurrence at 8 years: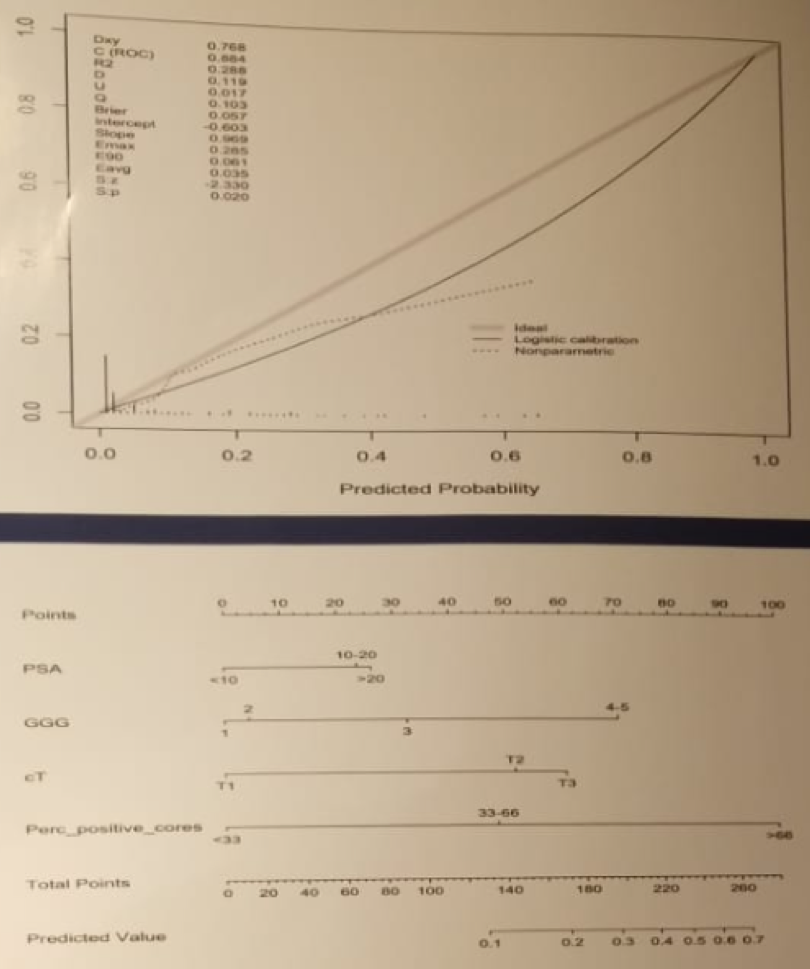
Figure 2 – Decision curve analysis comparing the accuracy of the novel risk tool presented in this study vs. the D’Amico risk classification and the CAPRA score: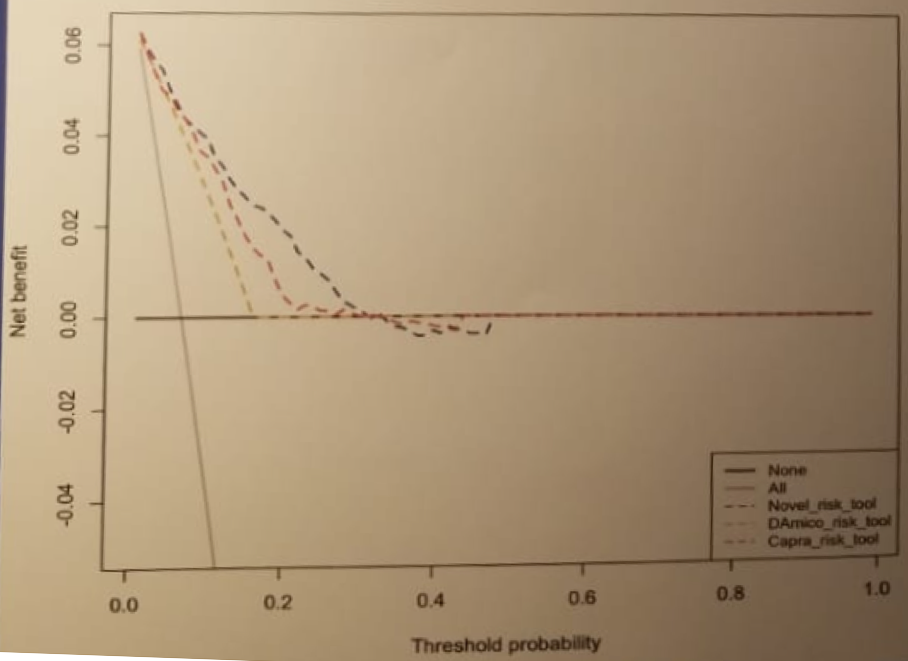
Table 2 – Nomogram derived risk score: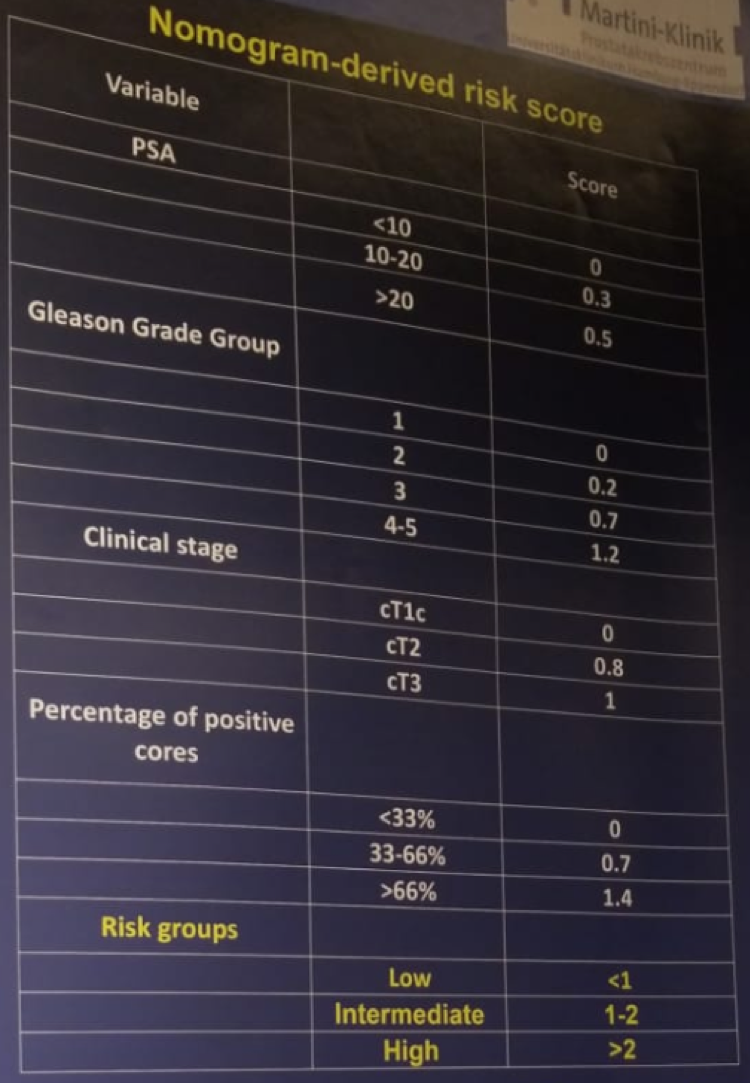
Figure 3 – Kaplan Meier plot depicting clinical recurrence-free survival stratified by nomogram derived risk groups:
In conclusion, the authors state that they have developed and externally validated a novel preoperative risk tool to predict long term recurrence in prostate cancer patients treated with radical prostatectomy. This model exhibited higher accuracy as compared to the available tools in the prediction of clinical recurrence at long term follow-up. This could potentially assist physicians in preoperative counseling and treatment decisions.
Presented by: Elio Mazzone, MD, San Raffaele Scientific Institute, Vita-Salute University San Raffaele, Urology, Milan, Italy
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.


