Barcelona, Spain (UroToday.com) Over the last several years, 68Ga-PSMA PET-CT has emerged as a modality for detecting metastatic lesions in the setting of biochemical recurrence for prostate cancer 1. At the Prostate Cancer Imaging from Diagnosis to Monitoring session at EAU 2019, Dr. Lopci and colleagues discussed their findings regarding the utilization of 68Ga-PSMA PET for the primary diagnosis of prostate cancer. The current study was designed to test the hypothesis that prostate biopsy using 68Ga-PSMA PET/Trans Rectal Ultrasound (TRUS) fusion images may have a clinical impact in the subset of patients with a high suspicion of prostate cancer, a previously negative biopsy and contraindications to or negative mpMRI.
This prospective study was performed at a tertiary high-volume hospital in order to use 68Ga-PSMA PET/CT in a selected subgroup of patients for diagnosis of primary prostate cancer. Men were considered eligible if they had a persistently elevated PSA and/or PHI (prostate health index) suspicion for prostate cancer, negative digital rectal examination, and at least one negative biopsy. The cohort comprised patients with either an equivocal mpMRI (PIRADS v2. ≤2) or an absolute or relative contraindication to mpMRI. All patients underwent whole body68Ga-PSMA PET/CT 60 minutes after radiopharmaceutical injection (185-250 MBq). Focal PSMA uptake superior to background activity was considered for the analysis and outlined for target biopsy. As follows is a figure corresponding to 68Ga-PSMA PET activity in the prostate: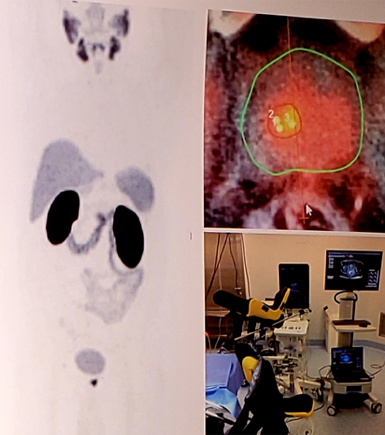
Semi-quantitative measures for all lesions comprised SUVmax and SUVratio-to-background. Sensitivities, specificities, and accuracy were calculated compared to histopathology results.
There were 88 cases referred for 68Ga-PSMA PET/CT. Of these, 66 patients (75%) had already performed mpMRI with either a negative result for prostate cancer (n=28) or positive mpMRI but a negative biopsy. In this subset of patients, 54 cases (61%) were addressed to 68Ga-PSMA PET/TRUS fusion biopsy that demonstrated the presence of 33 malignant lesions:
- 14 cases with GS 6 (3+3)
- 19 cases with GS 7 (15 cases GS 3+4; 4 cases GS 4+3)
- 2 cases GS 10 (5+5).
This study requires external validation. Cost-effectiveness analyses, particularly as it pertains to the overdiagnosis of non-clinically significant prostate cancer, will be important to assess especially in jurisdictions where 68Ga-PSMA PET is more expensive.
The authors concluded that in patients with a high suspicion of prostate cancer, despite previously negative biopsy and/or mpMRI, 68Ga-PSMA PET/CT is capable of detecting malignant lesions and identify with a high sensitivity clinically relevant prostate cancer.
Presented by: Egesta Lopci, Istituto Clinico Humanitas IRCCS Clinical and Research Hospital, Department of Nuclear-Medicine, Rozzano, Italy
Written By: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia Twitter: @zklaassen_md at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.
References:
- Perera M, Papa N, Christidis D, et al. Sensitivity, specificity, and predictors of positive 68GA-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: A systematic review and meta-analysis. Eur Urol 2016;70(6):926-937.


