Importantly, counting bone metastases to classify metastatic burden is limited by inter-observer variations and does not account for volume or coalescence. Automated bone scan index is a quantitative method of evaluating bone metastatic burden in a standardized and reproducible manner. At the Prostate Cancer Imaging from Diagnosis to Monitoring session at EAU 2019, Dr. Ali and colleagues presented results of their study evaluating in an exploratory fashion whether automated bone scan index can be used as a predictive imaging-based biomarker to define a mHNPC population which would benefit from prostate radiotherapy.
For this study, baseline bone scans of patients randomized to standard of care + prostate radiotherapy (STAMPEDE arm H) or their equivalents on the standard of care only (STAMPEDE arm A) were centralized. Scans meeting the DICOM and pixel compression requirements were evaluated in 2018 to calculate an automated bone scan index using the Exini automated bone scan index v3.2.1 software. This includes three steps:
- The skeleton is divided into 12 regions
- Artificial neural network based algorithm classifies hotspots as metastasis or benign
- Automated bone scan index is then calculated based on the area of metastasis, the area of the anatomical region in which it is located and a coefficient based on the proportion of total skeletal mass
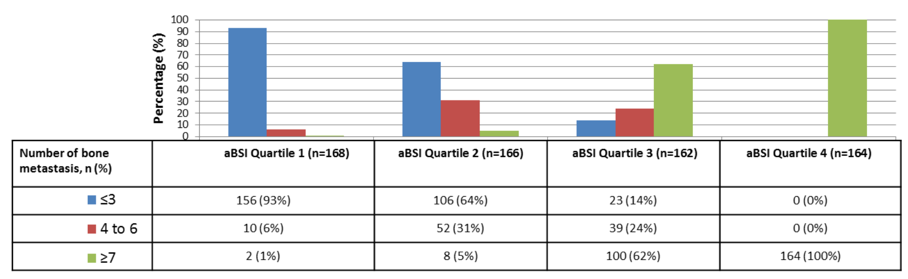
The M1/RT comparison included 2,061 patients, of which bone scans for 660 patients (arm A: 323; arm H: 337) met the software requirements for automated bone scan index calculation. The median age was 68 years, median PSA 100 ng/ml, and median automated bone scan index 0.9 (range 0-27.6). There were 595 (90%) men with bone metastasis and median follow-up was 39 months. Randomizing stratification factors and automated bone scan index were balanced between the arms. The authors found that bone metastasis counts were correlated to automated bone scan index (rho=0.88, p<0.001):
Both, the MFPI and STEPP analysis showed significant interaction of treatment with automated bone scan index for OS and FFS. Prostate radiation therapy improved OS (HR 0.50, 95%CI 0.28-0.91) and FFS (HR 0.35, 95%CI 0.22-0.54) in the lowest automated bone scan index quartile. OS and FFS benefits were not observed in the other automated bone scan index quartiles. The forest plot is as follows:
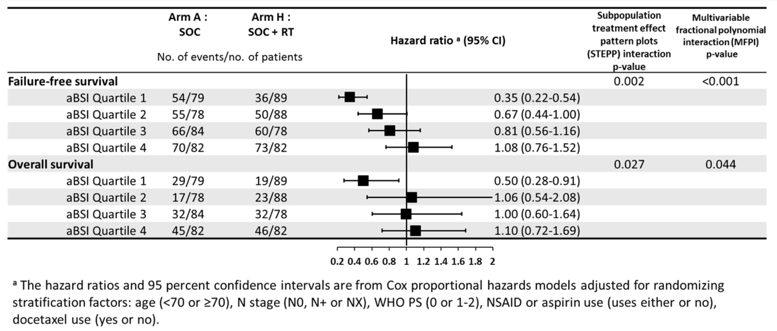
The authors concluded that manually counted bone metastasis on conventional bone scans positively correlates with the standardized and reproducible automated bone scan index. Furthermore, the addition of prostate radiation therapy to standard of care improved overall and failure-free survival in patients with the lowest automated bone scan index quartile. Automated bone scan index can be further evaluated as a predictive imaging-based biomarker for selecting newly diagnosed metastatic prostate cancer patients for prostate radiotherapy.
Presented by: Adnan Ali, University of Manchester, Genito-Urinary Cancer Research Group, Manchester, United Kingdom
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia, Twitter: @zklaassen_md at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.
References:
1. Parker CC, James ND, Brawley CD, et al. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): A randomized controlled phase 3 trial. Lancet 2018 Dec 1;392(10162):2353-2366.


