The Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) database, initiated by UCSF, is one of the older prospective longitudinal multi-institutional databases with the longest follow-up for localized prostate cancer. It includes over 15,000 men with prostate cancer from 43 mostly community programs. As such, in this abstract, the authors provide an update on prostate cancer-specific mortality outcomes after RP, brachytherapy (BT), EBRT, primary androgen deprivation therapy (ADT) and monitoring (WW/AS). This comes on the heels of updated data from large randomized studies publishing their long-term follow-up.1-3 In all of these studies, PCSM was low regardless of treatment modality used – but some studies suggested a benefit to surgery over monitoring.
The CaPSURE dataset included 11,719 men with localized prostate cancer and at least 6 months follow-up. Prostate cancer risk was assessed using the Stephenson pre-operative nomogram and the Cancer of the Prostate Risk Assessment (CAPRA) score (primarily used by UCSF, but validated in multiple studies). Following an initially descriptive look at long-term outcomes, multivariable analysis was performed to compare PCSM by primary treatment adjusting for age and case-mix.
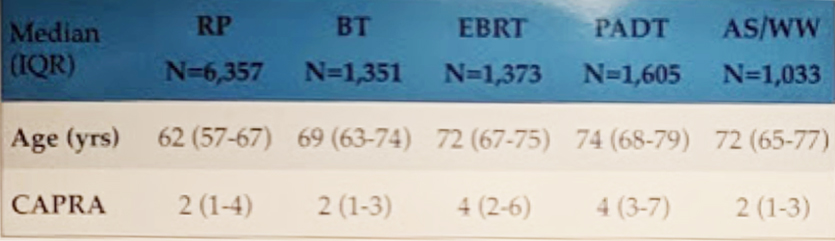
Of the 11,719 men, 6357 underwent RP, 1351 BT, 1,373 EBRT, 1605 PADT, and 1033 AS/WW. Basic demographics of the cohorts can be seen below:

In terms of oncologic outcomes, specifically PCSM, during the 18-year follow-up period, 493 men (4%) died from prostate cancer. First off, this is quite reassuring for men to see! PCSM is relatively low for men with localized prostate cancer.
Median months to PCSM was 85 months – or ~7 years (IQR 52-127 months). Adjusting for clinical CAPRA score the hazard ratios for PCSM relative to RP (which had the best PCSM) for BT, EBRT, PADT and AS/WW were 1.46 (p=0.049), 1.79 (p<0.01), 2.76 (, p<0.01), and 1.81 (p<0.01), respectively. The separation is best seen in the curves below:
Two additional analyses using 100-Kattan score and a de novo model demonstrated similar results.
Ultimately, the take-home message here is that:
- In low-risk patients, no specific treatment modality showed a significant prostate-cancer-specific survival benefit over other treatments
- Primary ADT does not provide any major benefit – and is not recommended for localized PCa anymore
The best we can say is that primary ADT is not beneficial and that men with low-risk disease do pretty well with most of the treatment modalities.
Presented by: Annika Herlemann, MD, Assistant Professor of Urology, the University of California, San Francisco, California, United States
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @JEFFUrology) at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.
References:
- Hamdy FC et al. “10-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Localized Prostate Cancer.” N Engl J Med. 2016 Oct 13;375(15):1415-1424. doi: 10.1056/NEJMoa1606220. Epub 2016 Sep 14.
- Wilt TJ et al. “Follow-up of Prostatectomy versus Observation for Early Prostate Cancer.” N Engl J Med. 2017 Jul 13;377(2):132-142. doi: 10.1056/NEJMoa1615869. N Engl J Med. 2018 Dec 13;379(24):2319-2329. doi: 10.1056/NEJMoa1807801.
- Bill-Axelson A et al. “Radical Prostatectomy or Watchful Waiting in Prostate Cancer - 29-Year Follow-up.”


