Often used as a benchmark for surgical skill, PSM rates are expected to be low in men with localized disease. Yet, as we all know, surgical skill varies greatly, especially as an increasing number of surgeons with varying levels of experience are completing robotic prostatectomies. Leveraging the NCDB, the authors evaluated 45,426 men from 1,152 institutions with pT2 prostate cancer and known margin status following radical prostatectomy (RP) over a 6 year period (2010-2015). Patient demographics and comorbidity, socioeconomic status, geographical and institutional information, cancer-specific variables and type of surgical approach were extracted. A multilevel hierarchical mixed-effects logistic regression model was performed to determine the factors associated with a risk of PSM and their contribution to a PSM status.
It should be noted that while PSM may serve as a benchmark for surgical skill and has some important prognostic value, it is still a short-term surrogate for longer term oncologic outcomes. NCDB, unfortunately, cannot assess cancer-specific survival but can look at overall survival. The authors do NOT focus on these outcomes in this abstract.
Baseline demographics can be found below for the entire cohort were provided in a very large table, that would not be able to clear if posted. However, suffice it to say that these were not well matched groups, with important differences in patient, surgeon/facility and tumor-related characteristics.
Median PSM rate was 8.5% (IQR: 5.2-13.0%, range: 0-100%), which is reasonably low.
On multivariable analysis, the features associated with lower PSM were:
- Robotic (OR: 0.90, 95% CI: 0.83-0.99) and laparoscopic (OR: 0.74, 95% CI: 0.64-0.90) surgical approach – these may be due to patient selection in the United States, as very few men undergo open prostatectomy unless for more advanced disease. However, it may also be a reflection of surgical facility.
- Academic institution (OR: 0.87, 95% CI: 0.76-1.00)
- High institution surgical volume (>297 cases [OR: 0.83, 95% CI: 0.70-0.99) – many studies (including some other abstracts in this session) have noted an association with surgeon experience and volume with surgical outcomes
- East North Central USA (OR: 0.71, 95% CI: 0.52-0.96)
On the other hand, race – specifically black men (OR: 1.13, 95% CI: 1.01-1.26) - and adverse cancer specific features (PSA 10-20, PSA >20, cT3 stage, Gleason 7, 8, 9-10; all p>0.01) were independently associated with a higher PSM. While black men have been known to have more advanced disease than their white male counterparts, anecdotally, the anatomy of the pelvis may contribute to these surgical outcome differences. It makes sense that men with worse pathology would have higher PSM rates.
The full hierarchical model is seen below:
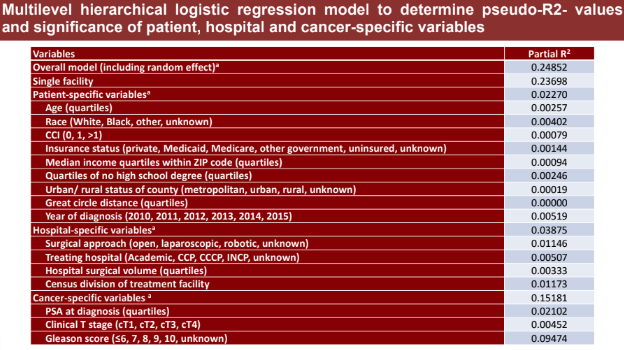
The overall multilevel hierarchical logistic regression model accounts for 24.9% of PSM variation. Patient-specific, institution-specific and cancer-specific factors accounted for 9.1%, 15.6% and 61.1% of the variation within the overall regression model respectively.
- It would appear that institution-specific factors only account for 15% of the variation, indicating that the institution may not be a major contributor to surgical outcomes
- However, as seen in the figure below, there is clearly a component of hospital ranking and surgical outcomes:
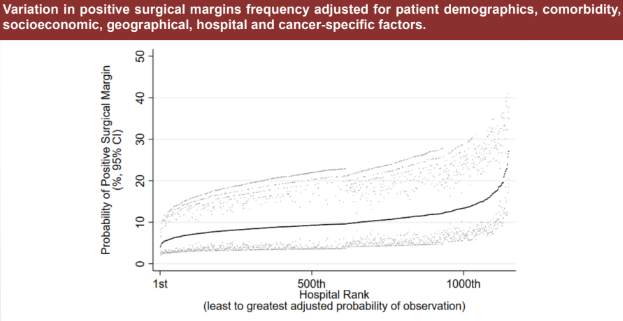
The majority of programs appear to be on the central plateau, however, albeit with a few outliers at either end.
The authors note that this may be an area for policymakers to concentrate future efforts to provide more standard care across the board.
Presented by: Wei Shen Tan, Center for Surgery and Public Health, Division of Urological Surgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusettes, USA, Division of Surgery & Interventional Science, University College London, London, United Kingdom, Department of Urology, Imperial College London, London, United Kingdom
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @JEFFUrology) at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.


