However, more recently, a subset of patients with oligometastatic disease is increasingly being recognized – and even men with clinically node-positive disease (with very low volume metastatic disease elsewhere) are being offered cytoreductive prostatectomy as part of the clinical trial. We know from the Messing data and others that a subset of men with pN1 disease following RP do well without any systemic therapy. Yet, better knowledge of the long-term outcomes of these patients is useful in understanding the natural history of these patients.
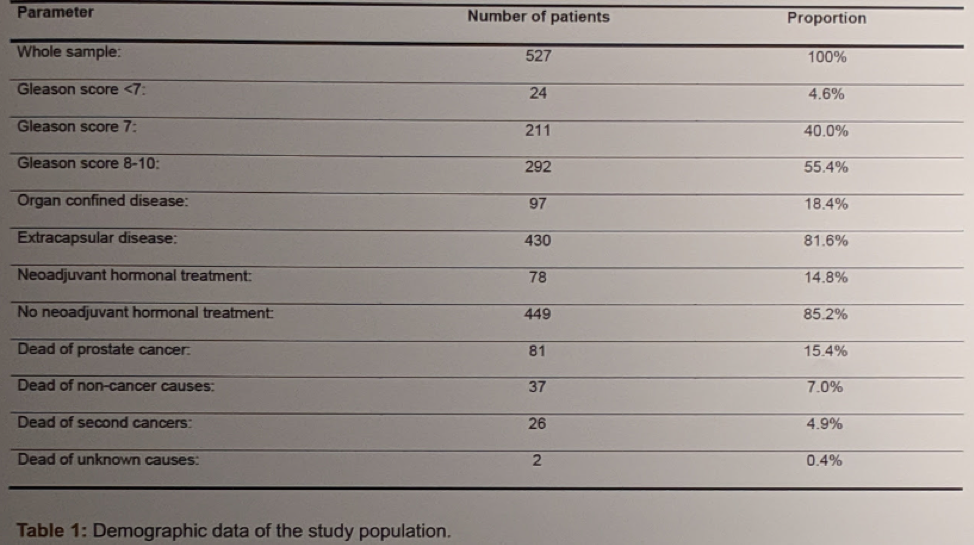
In this single-institution retrospective study, the authors provide long-term data regarding men who were node-positive at the time of radical prostatectomy. Of nearly 6000 men who underwent RP at their institution over a 22 year period, 527 were identified with positive lymph nodes on final pathology and were included in this analysis. The mean number of removed lymph nodes was 15. The mean follow-up in the surviving patients was 9.9 years. Full demographic data is below:
Variables considered in their analysis included: age (continuous variable), year of surgery (continuous variable), Gleason Score (<8 versus 8-10), local tumor stage (extracapsular disease versus organ confined), PSA level (<10 ng/ml versus higher or neoadjuvant hormonal therapy), lymph node density (number of involved lymph nodes per number of removed lymph nodes; continuous variable, per 10% increase), lymph node count (continuous variable), and the number of positive lymph nodes (continuous variable).
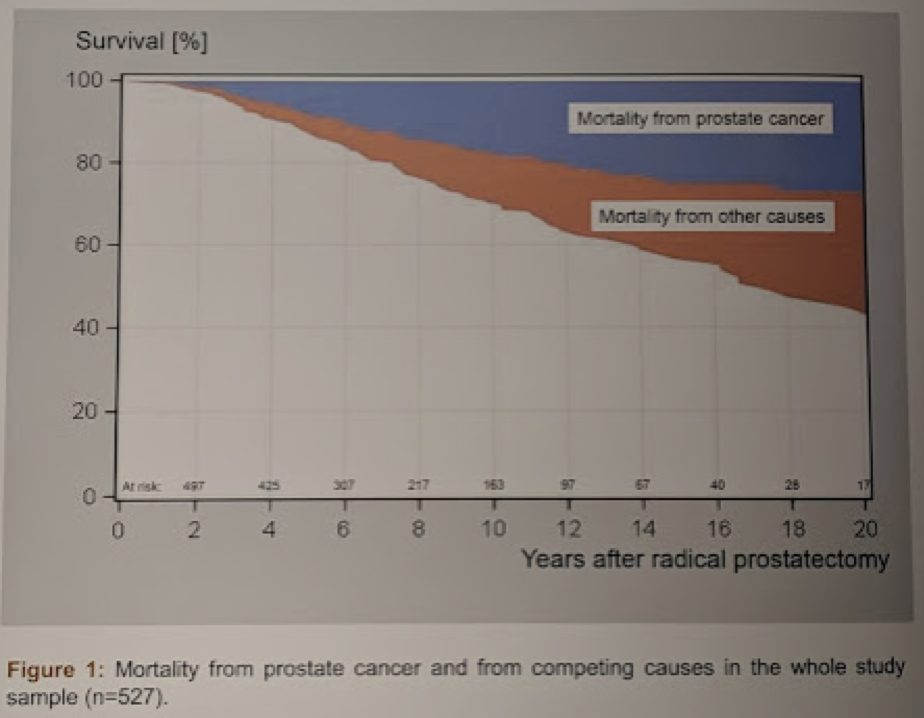
After 20 years, 28% of patients (95% confidence interval, CI, 20-36%) died from non-prostate cancer (competing) causes, whereas 29% (95% CI 23-36%) died from prostate cancer. This is consistent with prior studies, and reassuring that men with pN+ disease who are completely treated surgically have a 60-70% chance of durable CSS.
The survival outcomes are listed below:
Lymph node density (per 10% increase, hazard ratio, HR, 1.2, 95% CI 1.0-1.3, p=0.0056) and Gleason score (8-10 versus <8: HR 6.1, 95% CI 3.3-11.4, p<0.0001) predicted prostate cancer mortality. Patients with a Gleason score <8 and a lymph node density <median (11%) had a 20-year prostate cancer mortality of only 5%, whereas this rate in patients with Gleason scores 8-10 and a lymph node density >/=median was 44% (p<0.0001).
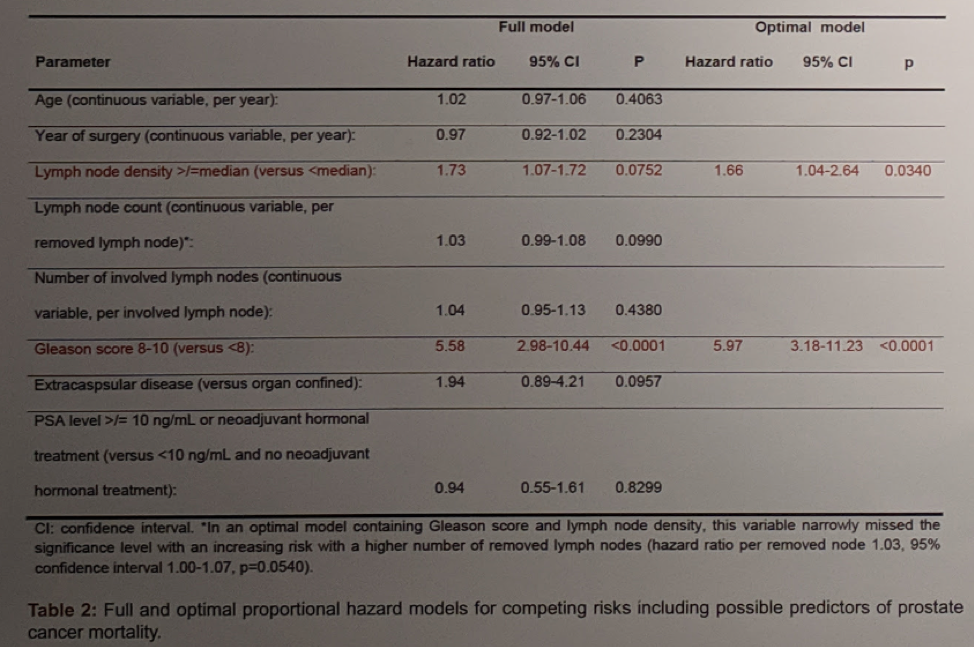
These likely reflect disease aggressiveness and disease burden, respectively. As such, these results make sense.
Overall, these results confirm those of prior studies, indicating that disease biology and tumor burden are the primary drivers of progression. However, a subset of men with oligometastatic prostate cancer to the nodes (with low disease burden and less aggressive tumors) may be cured with surgery alone.
Presented by: Michael Fröhner, MD, Department of Urology, Universität Dresden, Dresden, Germany
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @TjuUrology) at the 34th European Association of Urology (EAU 2019) #EAU19, conference in Barcelona, Spain, March 15-19, 2019.
References:
1. Messing EM, Manola J, Sarosdy M, Wilding G, Crawford ED, Trump D. Immediate hormonal therapy compared with observation after radical prostatectomy and pelvic lymphadenectomy in men with node-positive prostate cancer. N Engl J Med. 1999 Dec 9;341(24):1781-8.


