However, in men without known locally advanced disease prior to RP, nerve sparing (NS) may still be completed. In this study, the authors from two high volume centers in Europe evaluate the oncologic safety of NVB preservation in patients with pathological non-organ confined PCa at RP. This is a retrospective analysis, with its inherent biases. The authors identified patients who harbored pathologic T3 stage with bilateral or no NVB preservation at RP (single NS was not included), between 2000 and 2015. Only patients with Gleason grade group 3 or higher in the RP specimen and without lymph node invasion were included. These patients represented a higher risk cohort most likely to harbor pT3 disease and develop recurrence in the short term.
- Importantly, patients underwent NS at the discretion of the treating surgeon
- At the Martini Klinic, frozen sections are taken at the time of resection – if positive, NS is abandoned – and these patients are excluded from this analysis.
- At the University of Montreal, surgeons use clinical characteristics to guide NS
- Dr. Prasser noted that pre-operative staging studies may have been used, but were not used uniformly across all patients
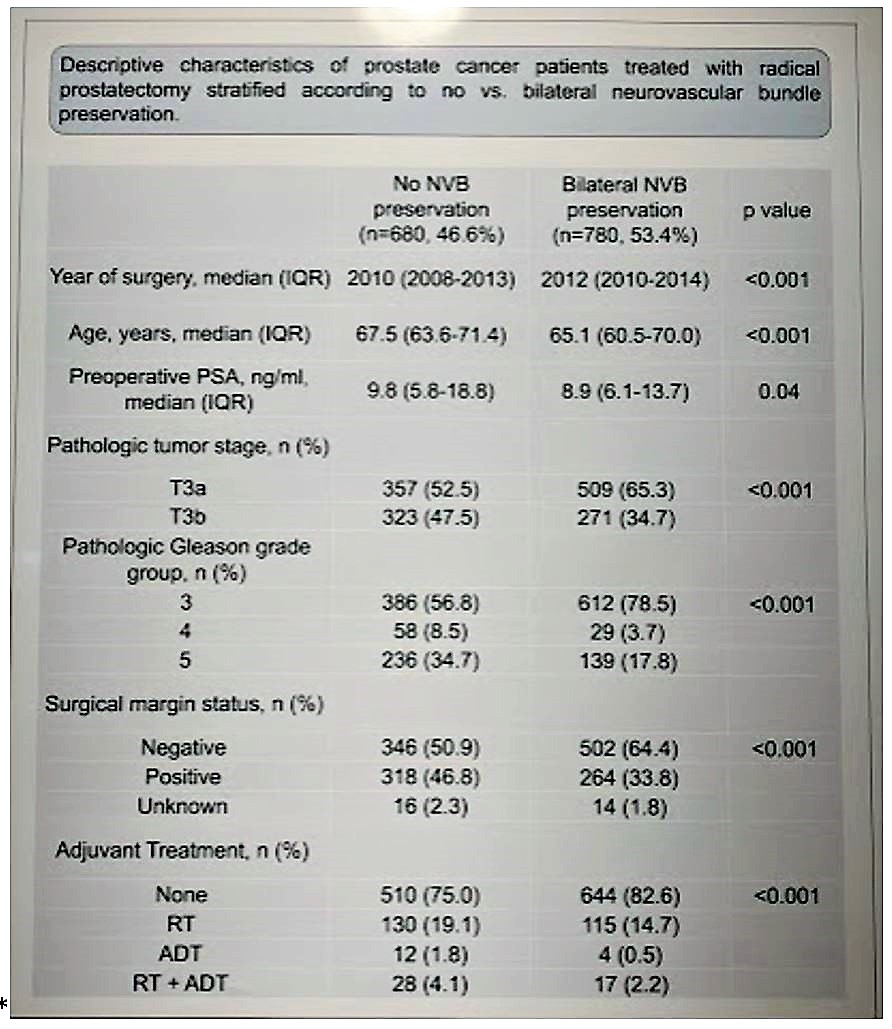
Of the 1,460 patients identified, 53.4% (780) underwent bilateral NVB preservation while the remainder had no NS – at the discretion of the treating physician.
When comparing the two groups, patients with bilateral NVB preservation had: lower surgical margin rate (33.8 vs. 46.8%, p<0.001) and less frequently harbored pathologic stage T3b (34.7 vs. 47.5%, p<0.001). This would suggest that they were selected out better for NS, but a significant portion still had PSM and pT3b disease. Full demographics shown below:
Median BCR-free survival after RP was 58.4 vs. 62.9 months (p=0.18), CR-free survival rates at 120 months (median not reached) were 76.9 and 71.9% (p=0.33) for bilateral and no NVB preservation, respectively.
On multivariable Cox regression models, after IPTW, NVB preservation was not an independent risk factor of BCR (p=0.7) or CR (p=0.7).
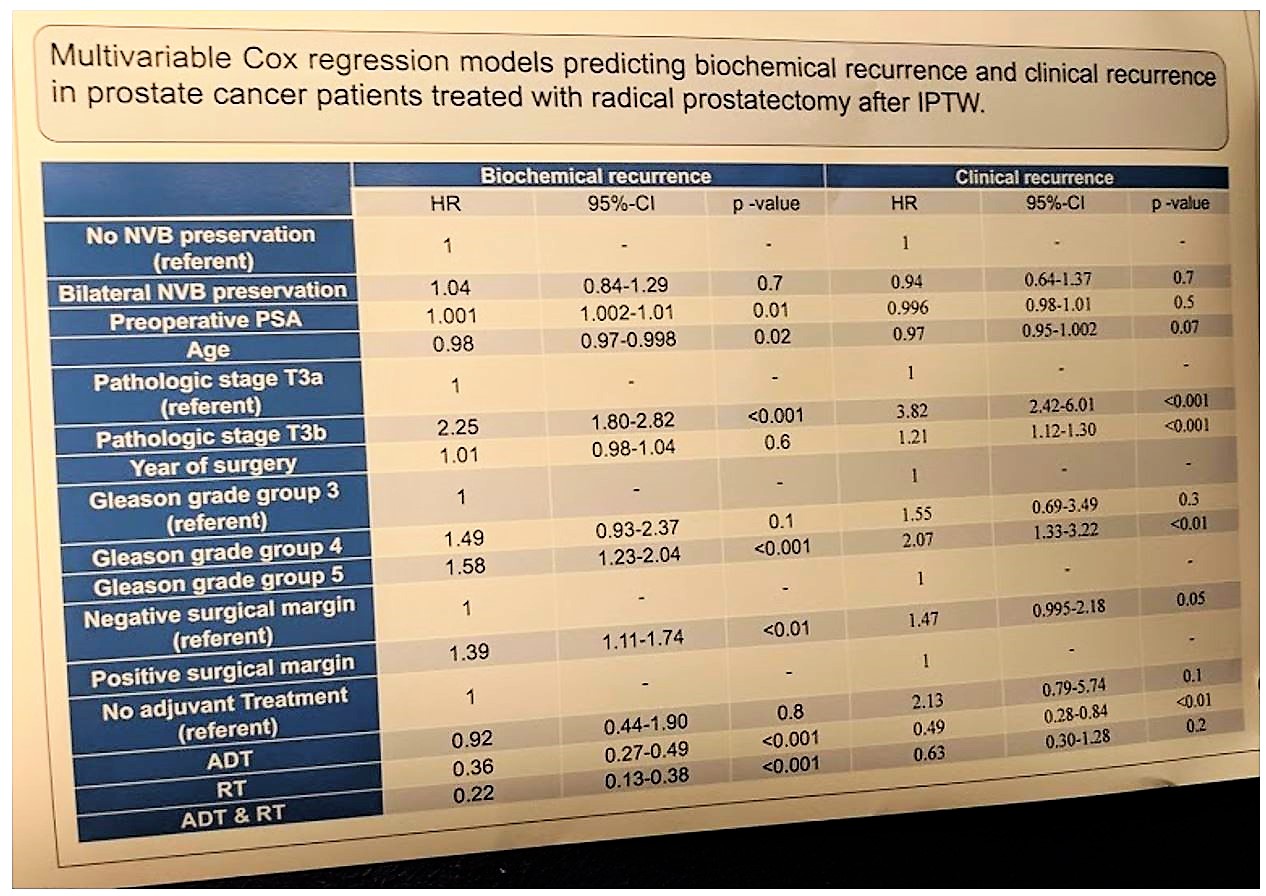
As can be expected, pT3b stage, year of surgery (and therefore experience), GG5 disease, PSM and RT / ADT use were predictors of BCR and CR.
Therefore, despite some selection bias, it would appear from this series that NS of bilateral NVB was not associated with worse oncologic outcomes – if appropriately selected. However, the article doesn’t comment on patient selection nor does it touch on unilateral NS. Knowing that patients at the Martini Klinik were selected out using frozen sections, perhaps this should be considered. Further data is required.
Presented by: Felix Preisser, MD, University Hospital Frankfurt, Dept. of Urology, Frankfurt, Germany
Written by: Thenappan Chandrasekar, MD, Clinical Instructor, Thomas Jefferson University, twitter: @tchandra_uromd, @TjuUrology at the 34th European Association of Urology (EAU 2019) #EAU19, conference in Barcelona, Spain from March 15-19, 2019.


