To assess this, they looked at their own single institution experience with RALP. They identified 2,857 prostate cancer patients treated with robot-assisted radical prostatectomy. The relationship between a surgeon’s prior experience (number of robotic prostatectomies performed before the patient’s operation) and the probability of positive surgical margins and biochemical recurrence was evaluated in regression models, adjusting for stage, grade, and PSA. They used BCR and PSM as their markers for oncologic outcomes, as they were the shortest time frame. However, as we know, these may not always reflect long-term oncologic outcomes.
The demographics of the cohort are as follows:
There were 9 total surgeons, and their experience is broken down as follows:
Total lifetime robotic prostatectomy experience:
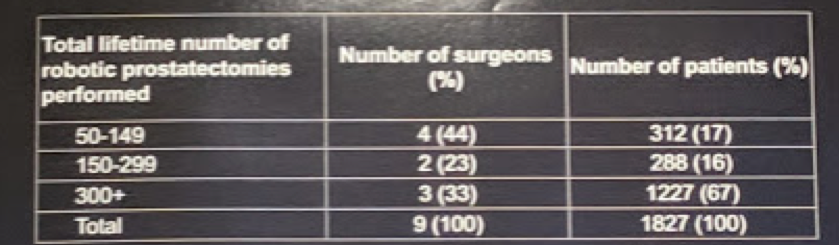
Annual volume:
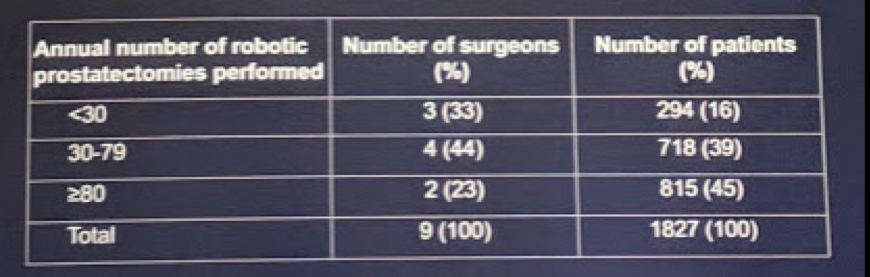
This represents a decent spectrum in terms of surgical experience.
The clinical and pathologic characteristics of the patients, broken down by surgeon experience:

No major differences in terms of case-mix were identified.
First looking at positive surgical margins: after adjusting for case mix (stage, grade, and PSA), the greater a surgeon’s experience was, the lower the probability of positive surgical margins (p=0.035). The risk of positive margins decreased from 15.3% to 6.7% for a patient treated by a surgeon with 10 and 250 prior procedures respectively (risk difference between 10 and 250 procedures 8.6%, 95%CI 2.3 to 12.8). In patients with a non-organ confined disease, the predicted probabilities of positive margins were 41.5% for patients treated by surgeons with 10 prior operations and 21.1% for patients treated by surgeons with 250 prior operations (absolute risk reduction 20.4%, 95%CI: -10.8 to 23.7). The figure below demonstrates this temporal association:

Yet, there is a slight rise after 250 cases that is not well explained…Unfortunately, Dr. Bravi could not easily supply a hypothesis for why this might be.
The relationship between surgical experience and the risk of biochemical recurrence after surgery was not significant (p=0.8), as seen below:
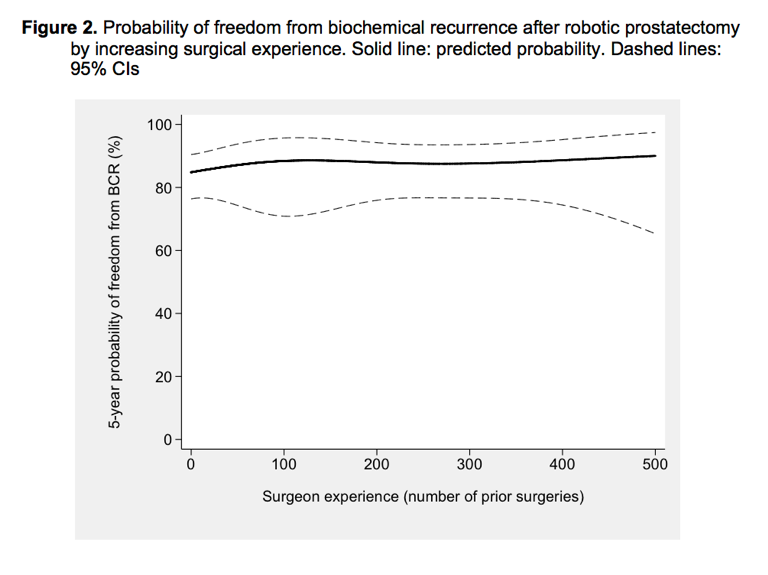
Based on this, the authors conclude that these results, which differ from prior studies focusing on open and laparoscopic prostatectomy, require further evaluation. However, one could posit that the learning curve is much shorter for a RALP due to the “intuitive” nature of the technology. Before making this assumption, further details in this study need to be clarified.
Presented by: Carlo Andrea Bravi, MD, IRCCS San Raffaele Hospital, Division of Oncology, Unit of Urology, Milan, Italy
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @TjuUrology) at the 34th European Association of Urology (EAU 2019) #EAU19, conference in Barcelona, Spain, March 15-19, 2019.


