This study took place between 2016 and 2018 and included 138 biopsy naïve patients with a suspicion of prostate cancer and a suspicious mpMRI lesion (>=PIRADS 3). All patients underwent in bore MRI targeted biopsies (2-5 cores per area) of suspicious lesions, without standard sampling. Out of 138 patients, 64 had subsequently undergone radical prostatectomy. The authors also performed a logistic regression model to assess predictors of discordance between biopsy and final pathology results (after radical prostatectomy).
The clinical characteristics of the patients are shown in table 1. Overall 19 (30%), 16 (25%), 4 (6.5%) and 2 (3%) of patients had clinically significant prostate cancer, extracapsular extension, seminal vesicle invasion, and lymph node invasion, respectively, at final radical prostatectomy pathology. Figure 1 demonstrates the concordance of tumor location and laterality between the biopsy and the final radical prostatectomy pathologic specimen, demonstrating an overlap of 86%. In contrast, the discordance rate in the Gleason score between the biopsy and the final radical prostatectomy specimen was as high as 44% (28/63 patients). A total of 3 and 23 patients had downgrading and upgrading, respectively. Lastly, 3 (5%) and 7 (11%) clinically significant prostate cancers were overestimated and underestimated, respectively, by performing biopsies only in the target zone. Table 2 demonstrates the results of the multivariable logistic regression model attempting to ascertain the predictors of discordance between the biopsy and radical prostatectomy pathology results. The results of this model show that rising maximal positive core length predicts discordance (OR 1.22 95% CI 1.03-1.06).
The authors concluded that approximately 50% of patients referred for mpMRI-targeted biopsy demonstrate a Gleason grade discordance between the biopsy and the final radical prostatectomy pathology results. Also, 11% of the patients are affected by clinically significant prostate cancer that is misdiagnosed if standard biopsy cores are avoided. These are very interesting results that require validation in larger prospective studies.
Table 1 – Clinical characteristics of patients:
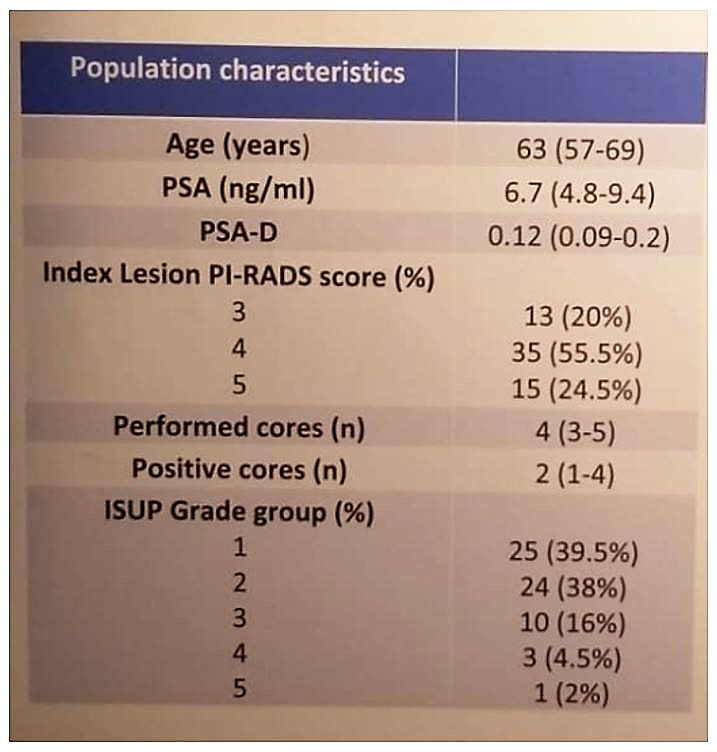
Figure 1 – Concordance rate between biopsy and radical prostatectomy final specimens:
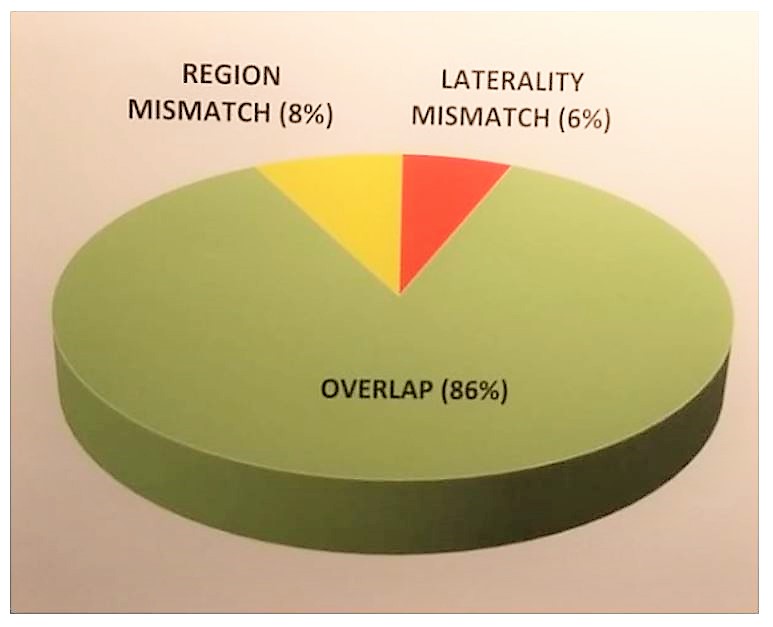
Table 2 – Logistic regression analysis:

References:
1. Kasivisvanathan, Veeru, et al. “MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis.” The New England Journal of Medicine, 19 Mar. 2018, doi:10.1056/NEJMoa1801993.
Presented by: Francesco Alessandro Mistretta, MD, Department of Urology, European Institute of Oncology, Milan, Italy
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre @GoldbergHanan at the 34th European Association of Urology (EAU 2019) #EAU19, conference in Barcelona, Spain from March 15-19, 2019.


