(UroToday.com) The 37th Annual European Association of Urology Congress held in Amsterdam, Netherlands between July 1st,and 4th 2022 was host to the 8th ESO Prostate Cancer Observatory: Innovations and Care in the Next 12 Months. Dr. Fanti was tasked with giving the imaging specialist’s perspective on prostate-specific membrane antigen (PSMA)-PET/CT.
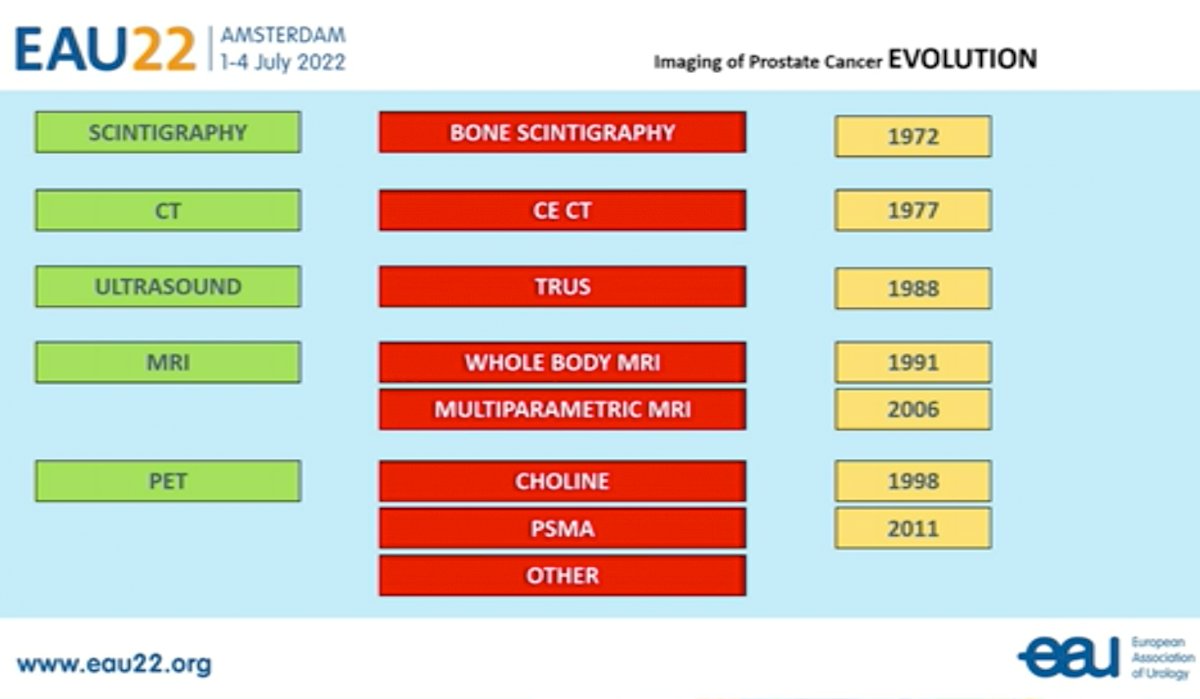
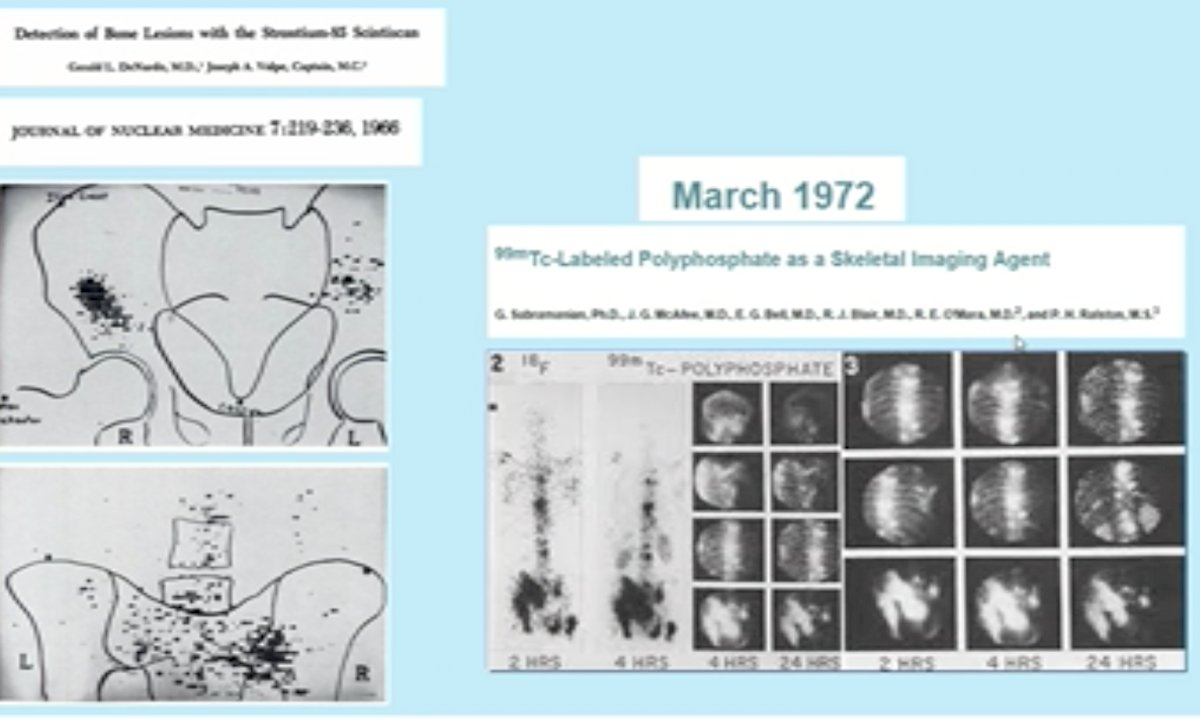
Dr. Fanti began his presentation by giving a historic overview of the evolution of prostate cancer imaging modalities since 1972. He notes that PSMA has been available since 2011, and he finds it fascinating that PSMA-based imaging modalities have taken so long to become widely adopted/accepted.
In addition to its improved diagnostic performance, from an imaging specialist’s perspective, PSMA imaging is much easier to interpret visually.
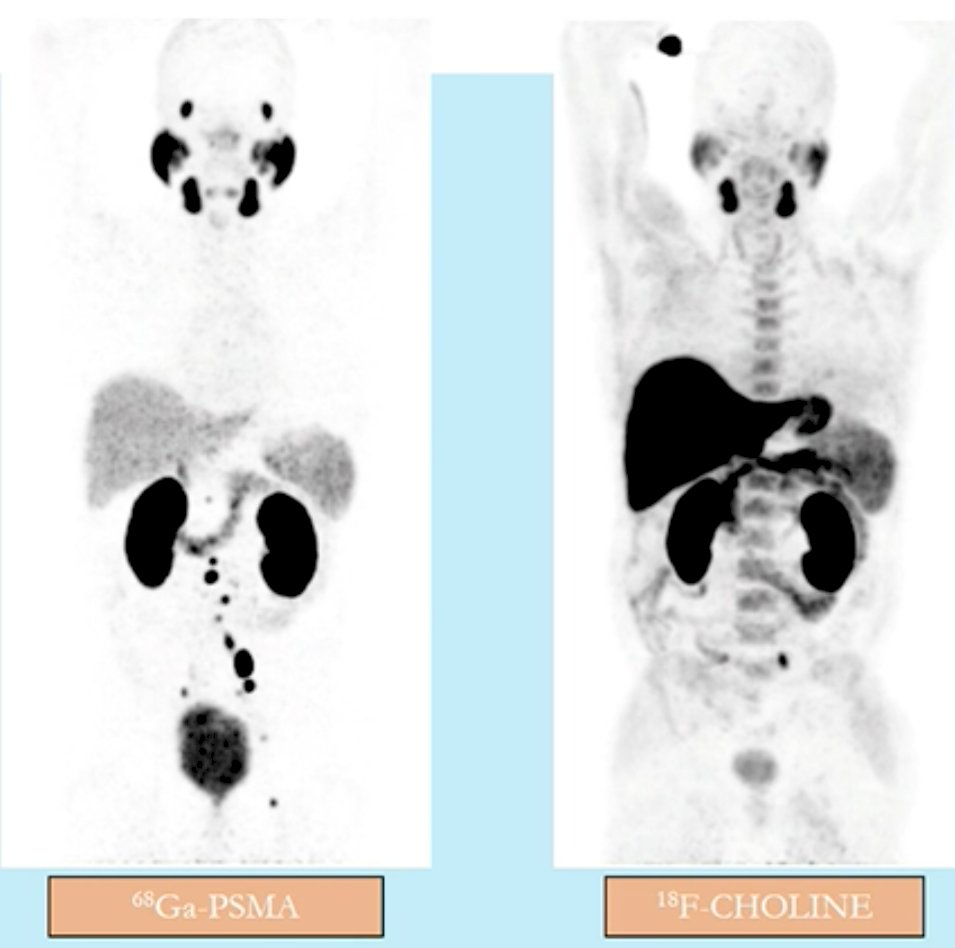
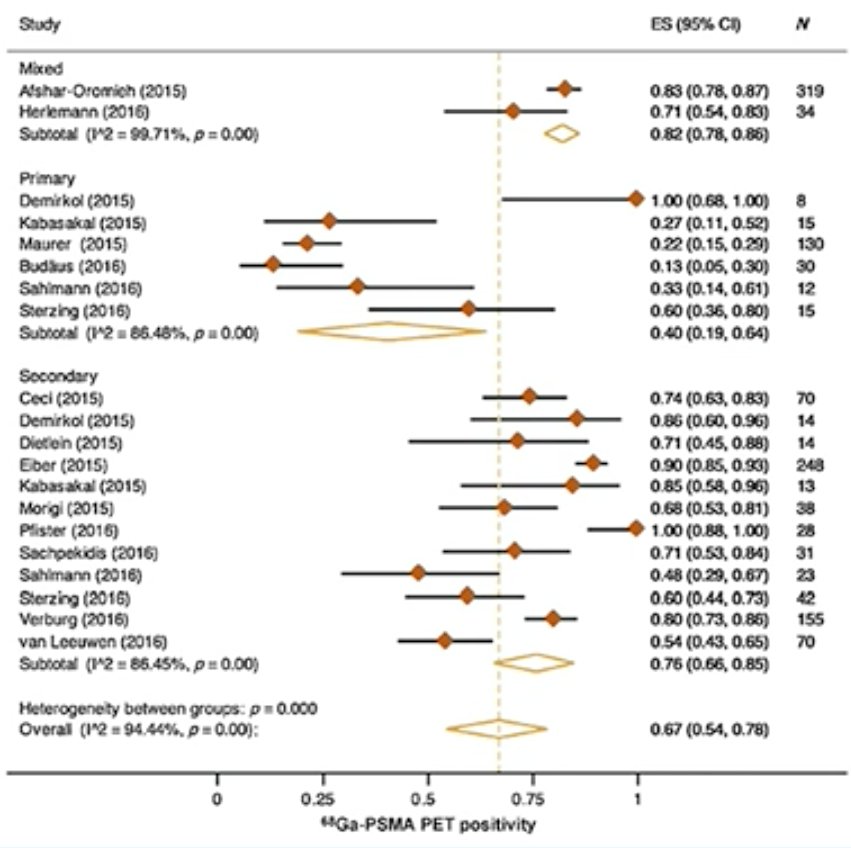
A 2016 systematic review by Perera et al. demonstrated that the summary sensitivity and specificity of 68Ga-PSMA testing was 86% for both. On a per-lesion analysis, the summary sensitivity and specificity were 80% and 97%, respectively.1
This improved diagnostic performance of PSMA PET imaging has been reflected in the most recent EAU Prostate Cancer guidelines which state that:
- PSA recurrence after radical prostatectomy: “Perform PSMA PET/CT if the PSA level is >0.2 ng/mL and if the results will influence subsequent treatment decisions.” (Weak Recommendation)
- PSA recurrence after radiotherapy: “Perform PSMA PET/CT (if available) or fluciclovine PET/CT or choline PET/CT in patients fit for curative salvage treatment” (Strong Recommendation)
- Staging for high-risk localized disease/locally advanced disease: “When using PSMA PET or whole-body MRI to increase sensitivity, be aware of the lack of outcome data of subsequent treatment changes.”
He notes that when the ASCO guidelines adopted PSMA imaging in their recommendations for men for whom salvage radiotherapy is contemplated, it was one of the few times where an imaging modality was recommended before it was approved in a country.
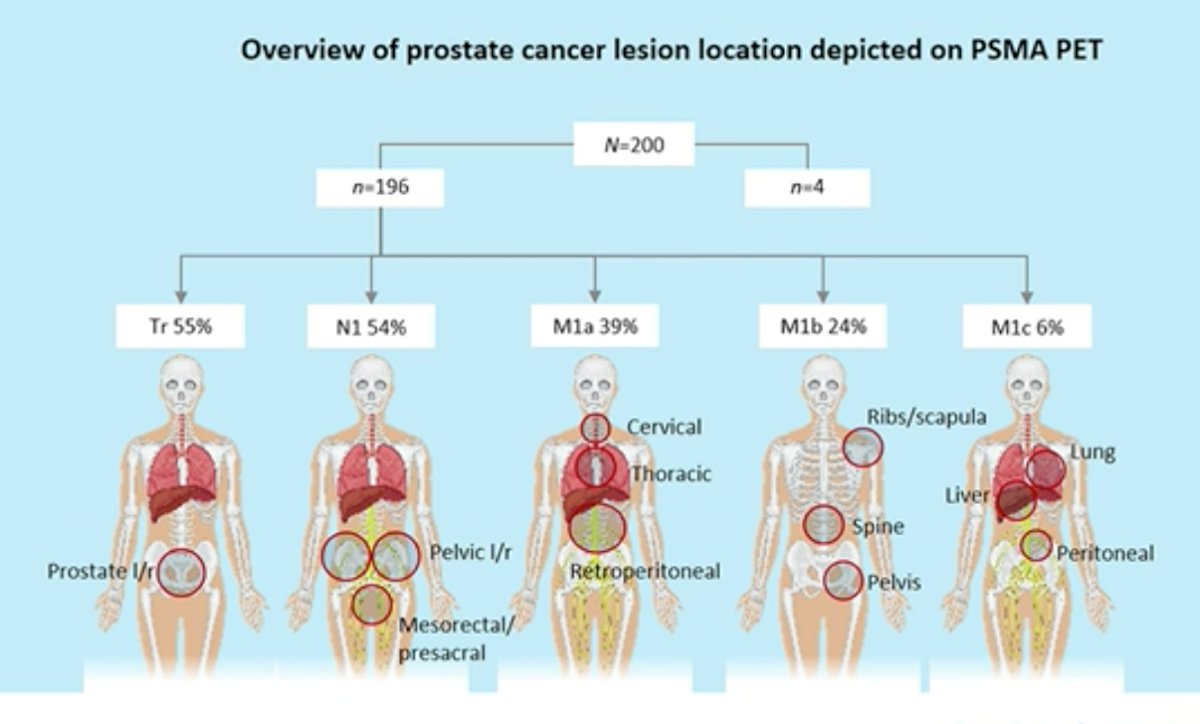
The emergence of PSMA PET/CT imaging also means the likely disappearance of the non-metastatic castration-resistant prostate cancer (\nmCRPC) disease space. Of 200 patients diagnosed with nmCRPC based on conventional imaging, 196 (98%) were found to have pelvic disease or distant metastases on PSMA PET/CT with 55% having M1 disease. New treatment was initiated after PSMA PET/CT in 62% of patients.2
Dr. Fanti went on to highlight a systematic review by his group on the role of imaging in early prostate cancer. 68Ga-PSMA PET/CT had higher detection rates than any other imaging modality, especially in patients with low PSA values (detection rates of 11.3-58.3% for PSA<0.2 ng/ml and 65.0% for PSA<0.5 ng/ml).3
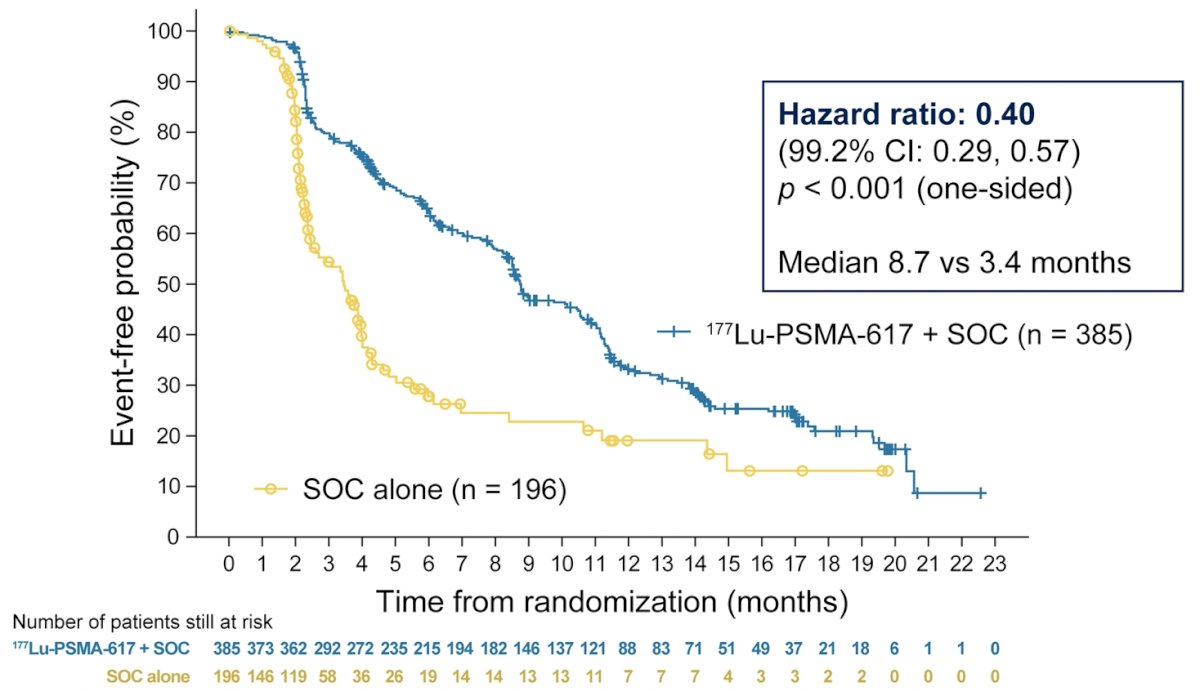
PSMA-based theranostics have also emerged as exemplified by the VISION trial that randomized patients previously treated with both >=1 androgen receptor pathway inhibitor and 1 or taxane regimens in a 2:1 fashion to receive either 177Lu-PSMA-617 (7.4 GBq every 6 weeks x 6 cycles) plus standard of care (SOC) or SOC alone. Over a median study follow-up of 20.9 month (as of a data cut-off of 27 January 2021), treatment with 177Lu-PSMA-617 + SOC significantly improved overall survival by a median of 4.0 months (median OS, 15.3 vs 11.3 months; HR, 0.62 [95% CI: 0.52, 0.74]; p < 0.001, one-sided), compared to SOC alone, in the overall cohort of all randomized patients (n=831).
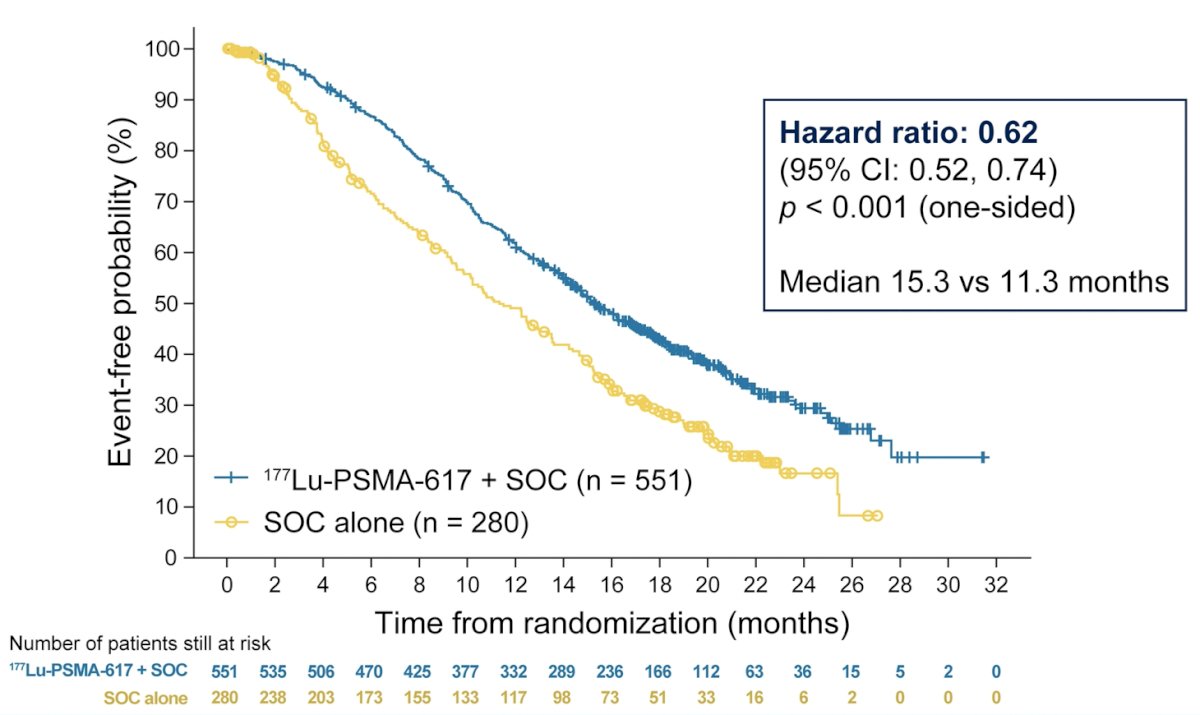
Treatment with 177Lu-PSMA-617 + SOC significantly improved rPFS by a median 5.3 months (median rPFS, 8.7 vs 3.4 months; HR, 0.40 [99.2% CI: 0.29, 0.57]; p < 0.001, one-sided).
Dr. Fanti concluded his talk with following points:
- >2,400 articles have been published in this disease space since 2012
- PET-based imaging is now incorporated into guidelines
- He hopes that PET-based imaging will be increasingly incorporated into randomized controlled trials
- The field of PSMA-based theranostics is developing quickly
Presented by: Stefano Fanti, MD, Professor, Department of Experimental, Diagnostic and Specialty Medicine, Universita di Bologna, Bologna, Italy
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2022 European Association of Urology (EAU) Annual Hybrid Meeting, Amsterdam, NL, Fri, July 1 – Mon, July 4, 2022.
References:
- Perera M, et al. Sensitivity, Specificity, and Predictors of Positive 68 Ga-Prostate-specific Membrane Antigen Positron Emission Tomography in Advanced Prostate Cancer: A Systematic Review and Meta-analysis. Eur Urol. 2016;70(6):926-37.
- Fendler WP, et al. Prostate-Specific Membrane Antigen Ligand Positron Emission Tomography in Men with Nonmetastatic Castration-Resistant Prostate Cancer. Clin Canccer Res. 2019;25(24):7448-54.
- De Visschere PJL, et al. A Systematic Review on the Role of Imaging in Early Recurrent Prostate Cancer. Eur Urol Oncol. 2019;2(1):47-76.


