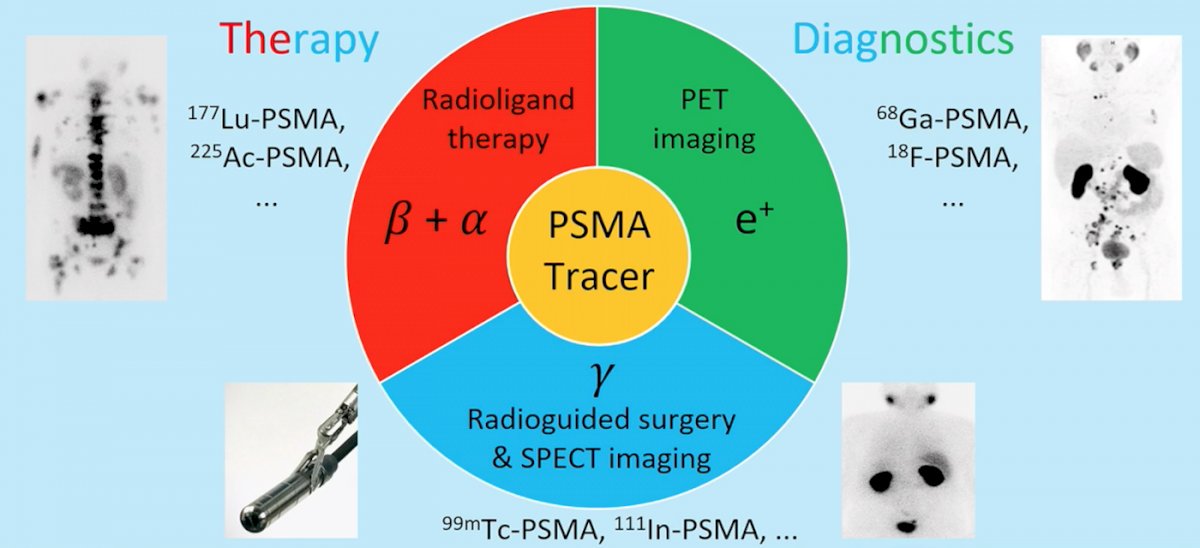
(UroToday.com) The 2022 EAU annual meeting featured a joint session of the EAU, EANM, ESMO, and ESTRO societies examining modern diagnostic and therapeutic approaches in prostate cancer, including a presentation by Dr. Tobias Maurer discussing surgery as a salvage treatment option for the PSMA avid lesion in the setting of recurrent prostate cancer. Salvage surgery for PSMA avid lesions has three potential uses, including local recurrence after non-ablative therapy, local recurrence after radical prostatectomy, and loco-regional lymph node metastasis. PSMA theranostics includes therapy and diagnostics, as highlighted in the following figure:
Salvage radical prostatectomy for local recurrence after non-ablative therapy (ie. radiotherapy) is feasible and can be enhanced by intraoperative histological assessments (NEUROSAFE-technique). More recently, PSMA tracers have been used for intraoperative margin assessment, utilizing a beta-probe for measurement or Cerenkov luminescence imaging after injection of 68-Ga-PSMA-11:
Dr. Maurer notes that the EAU guidelines state that salvage radical prostatectomy should be considered only in patients with low comorbidity, a life expectancy of at least 10 years, a pre-salvage surgery PSA < 10 ng/mL, initial biopsy ISUP grade <2/3, initial T1 or T2, and no lymph node involvement or evidence of distant metastatic disease.
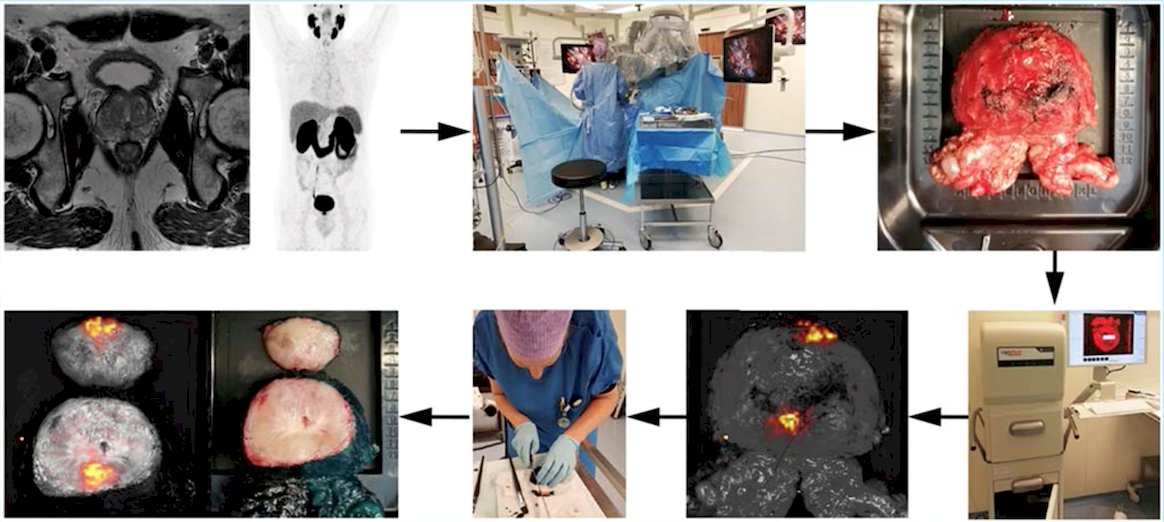
The challenge of salvage surgery is the intraoperative detection of small lymph nodes in the pelvis. One way to assist with detection is to use PSMA-radio-guided surgery, which includes a preoperative IV injection of 111In- or 99mTc-labeled PSMA-ligand and subsequently facilitates intraoperative detection of metastatic lesions by gamma probe:

In a study from Dr. Maurer’s group,1 40 patients were treated with open salvage surgery in two centers (2014-2020), with all patients presenting with biochemical recurrence after radical prostatectomy with a singular local recurrence at PSMA PET imaging. Among these patients, 33 (82.5%) received previous salvage radiation therapy. Prior to salvage surgery, the median PSA was 0.9 ng/ml (IQR 0.5–1.7 ng/ml), and postoperatively the median PSA nadir was 0.1 ng/ml (IQR 0–0.4 ng/ml). In 31 (77.5%) patients, clinical biochemical response was observed. Over a median follow-up of 24.4 months, 22 (55.0%) patients experienced biochemical recurrence and 12 (30.0%) received further therapy. At 1 year of follow-up, the biochemical-free survival rate was 62.2% and treatment-free survival rate was 88.3%:

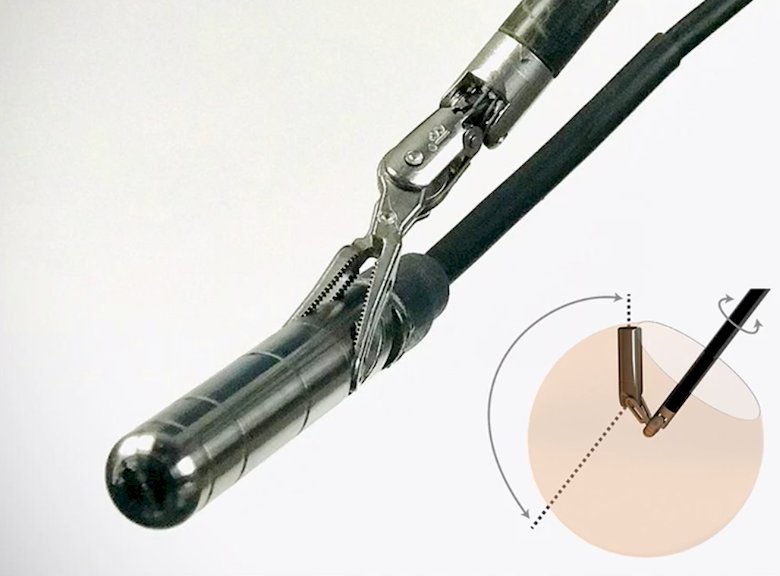
The previous studies discussed by Dr. Maurer were all open salvage procedures, however recently they have been able to use robotic surgery for salvage therapy based on the advent of a drop-in gamma probe to facilitate robotic minimally-invasive PSMA-radioguided surgery. This technology is compatible to standard gamma counters, re-sterilizable, inserted through a 12 mm assistant trocar, and maneuvered by the Prograsp allowing rotational freedom:
Dr. Maurer emphasized that the standard of care for local recurrence after radical prostatectomy is salvage radiotherapy. Additionally, re-salvage radiotherapy is reported in the literature, particularly after a long interval. However, local salvage PSMA radioligand surgery is a novel option, particularly after salvage radiotherapy.
But, does salvage lymph node dissection in prostate cancer make sense? Bravi et al.2 undertook a multi-institutional approach to assess these long-term outcomes, including 189 patients who experienced PSA rise and nodal-only recurrence after radical prostatectomy and underwent salvage lymph node dissection at 11 centers between 2002 and 2011. Recurrences were detected with either 11C-choline or 68Ga PSMA. The primary outcome was cancer-specific mortality, and the secondary outcomes were overall mortality, clinical recurrence, biochemical recurrence, and androgen deprivation therapy (ADT)-free survival after salvage lymph node dissection. There were 110 and 163 patients who experienced clinical recurrence and biochemical recurrence, respectively, with clinical recurrence-free and biochemical recurrence-free survival at 10 years of 31% and 11%, respectively. After salvage lymph node dissection, a total of 145 patients received ADT, with a median time to ADT of 41 months. Importantly, additional therapy was warranted in >60% of patients within 6 months of salvage lymph node dissection. At a median follow-up for survivors of 87 (IQR 51 to 104) months, 48 patients died, of which 45 died from prostate cancer. At multivariable analyses, patients who had PSA response after salvage lymph node dissection (HR 0.45; p = 0.001), and those receiving ADT within 6 months from salvage lymph node dissection (HR 0.51; p = 0.010) had a lower risk of death from prostate cancer.
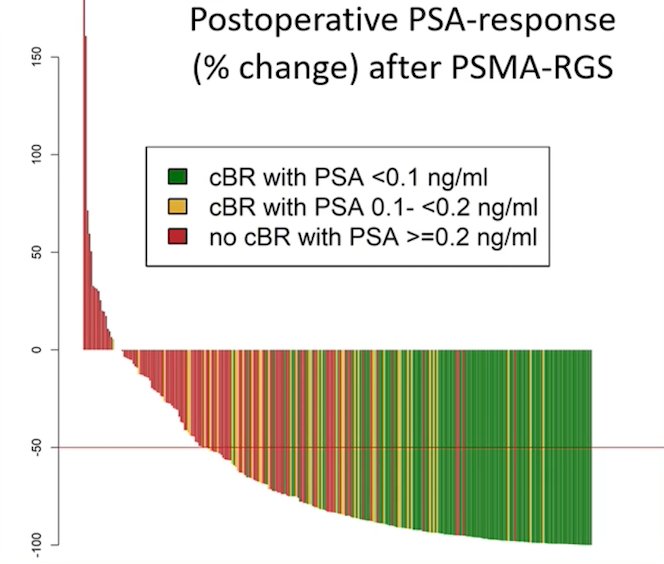
Dr. Maurer’s group recently presented their up to date cohort of patients undergoing salvage lymph node dissection via PSMA radioguided surgery at the 2022 GU ASCO meeting. Over the study interval, 364 eligible patients were identified. At the time of PSMA-radio-guided surgery, the median age and preoperative PSA was 67 (IQR 61-71) years and 1.0 (IQR 0.5-1.9) ng/ml. Metastatic soft-tissue lesions were removed in 356 (94.4%) patients. In general, surgery was well tolerated though, within three months of surgery, 25 (6.6%) patients experienced severe (grade 3-4) Clavien-Dindo complications. Most patients had a significant decrease in their PSA following surgery, with many becoming undetectable:
Over the course of follow-up, 235 patients experienced BCR and 129 patients received further therapy. As follows are the Kaplan-Meier curves for biochemical recurrence-free survival and treatment-free survival:
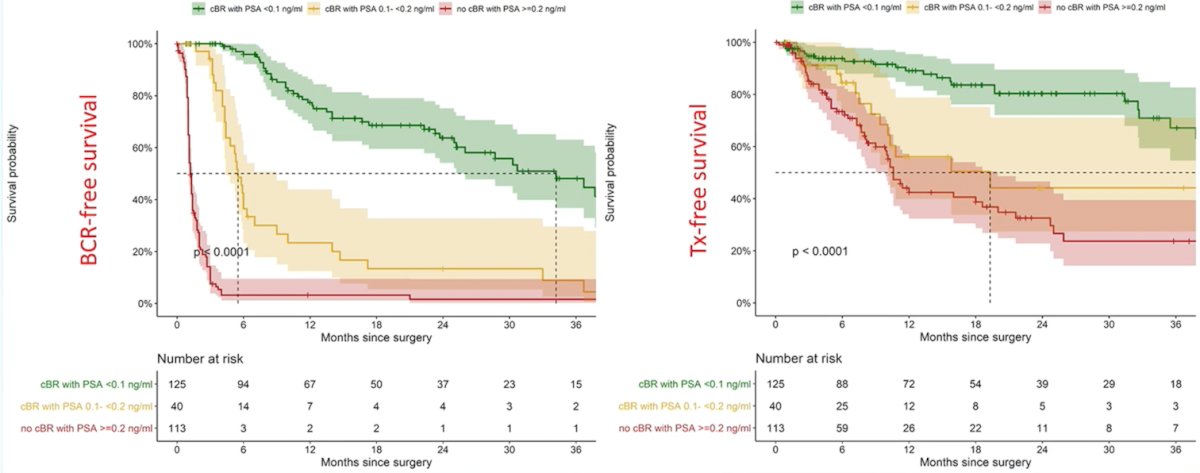
Using multivariable Cox models, higher preoperative PSA (HR: 1.06), a higher number of PSMA-avid lesions on preoperative imaging (HR: 1.2) and multiple (pelvic plus retroperitoneal) localizations (HR: 1.7), as well as retroperitoneal localization (HR: 2.0) of lesions in PSMA PET imaging were independent predictors of BCR after PSMA-radio-guided surgery.
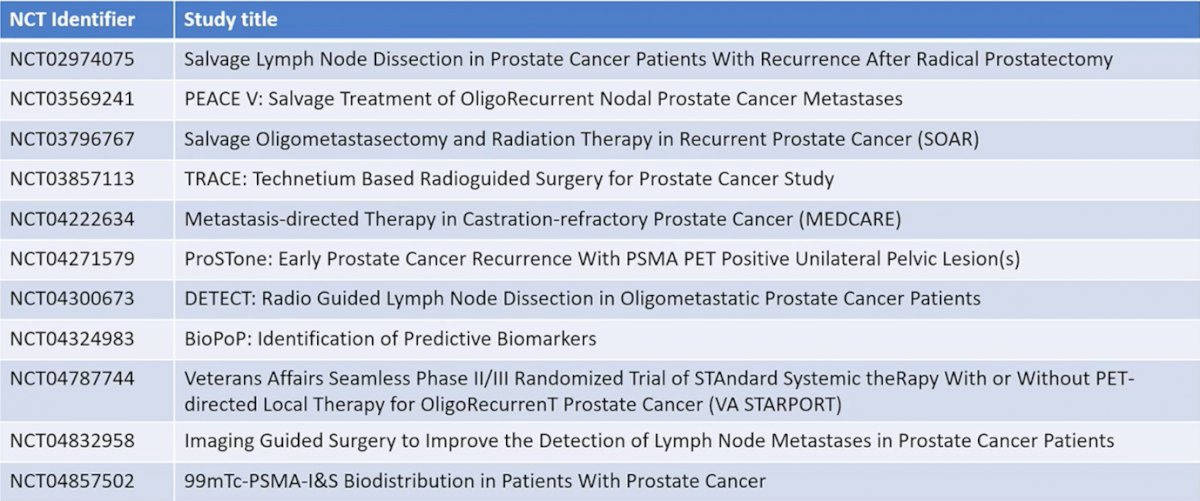
Dr. Maurer notes that there are further prospective studies to come:
For loco-regional lymph node metastasis, Dr. Maurer concluded that salvage lymph node dissection/PSMA-radioguided surgery represents an individualized treatment approach. Careful selection of patients is necessary, but oncological outcomes are promising, representing an additional option after or even prior to salvage radiotherapy.
Presented by: Tobias Maurer, MD, Martini-Klinik Prostate Cancer Center, University Hospital Hamburg-Eppendorf, Hamburg, Germany
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 European Association of Urology (EAU) Annual Hybrid Meeting, Amsterdam, NL, Fri, July 1 – Mon, July 4, 2022.
References:
- Knipper S, Ascalone L, Ziegler B, et al. Salvage surgery in patients with local recurrence after radical prostatectomy. Eur Urol. 2021 79:537-544.
- Bravi CA, Fossai N, Gandaglia G, et al. Long-term Outcomes of Salvage Lymph node dissection for nodal recurrence of prostate cancer after radical prostatectomy: Not as Good as Previously Thought. Eur Urol 2020 Nov;78(5):661-669.


