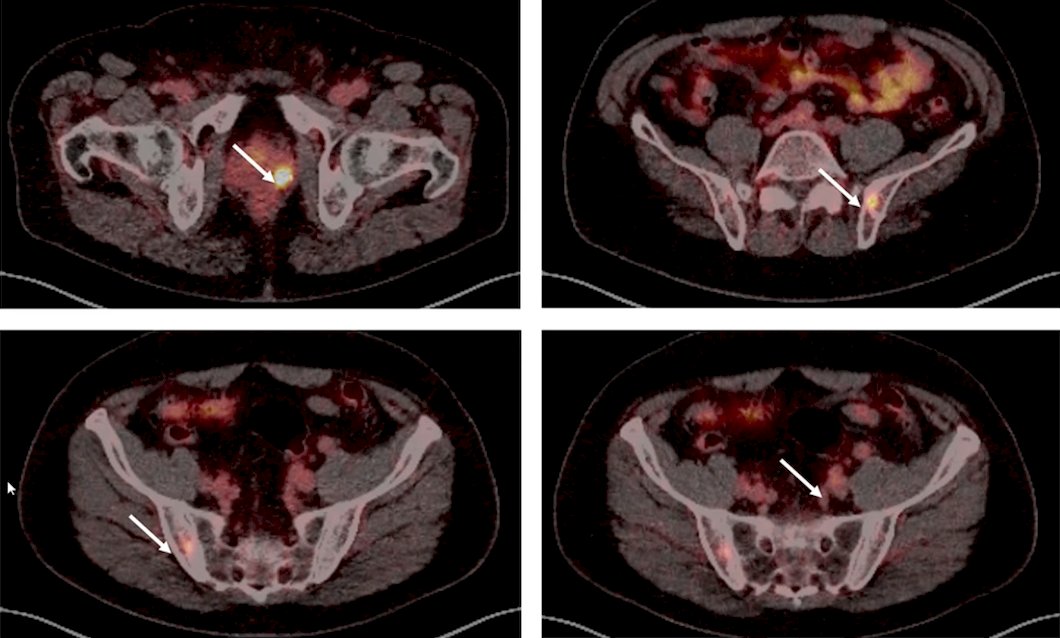
(UroToday.com) The 2022 EAU annual meeting featured a session on prostate cancer high-risk local treatment, including a presentation by Dr. Nicolas Mottet discussing that limited bone involvement detected by PSMA PET/CT is associated with palliative treatment. To start, Dr. Cladia Kesch from Germany presented a case for discussion. The patient is a 66 year old man with a PSA of 8.2 ng/mL, normal digital rectal exam, prostate volume of 60 mL, IPSS score of 11, and IIEF score of 25. His medical history included hypertension (treated with an ACE inhibitor) and obesity (BMI 30 kg/m2). He subsequently underwent a 12-core TRUS prostate biopsy that showed Gleason score 4+4 = 8 prostate adenocarcinoma in 4 out of 12 cores. His conventional imaging staging studies were negative (cN0M0), however his staging68Ga-PSMA-PET/CT suggested lymph node involvement and potentially oligometastatic bone involvement (cN1M1b):
Dr. Mottet then discussed why this clinical situation is palliative, which he argues is secondary to this being a systemic disease. Palliative means that there is at least minimal (if any) chance to cure (ie. no relapse during very long follow-up), but it does not mean that you are going to die in the next few months or even next few years. But, because we are dealing with a systemic disease in this case, Dr. Mottet notes that systemic prostate cancer is almost never cured. Furthermore, Dr. Mottet emphasized that false positives on staging studies do exist, mostly with 18F-PSMA and mostly in the ribs, which should be checked with conventional imaging (the associated CT). Another potential issue it the underestimation of the real extent of disease.
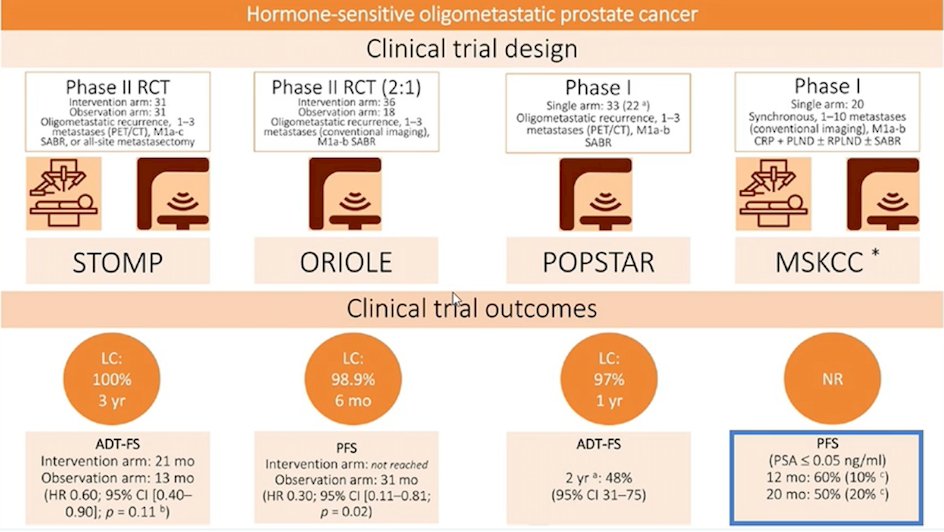
The only evidence for metastasis-directed therapy at relapse is from prospective cohorts, including 4 studies for a total of 158 patients (109 in the experimental arms), including the STOMP, ORIOLE, POPSTAR, and MSKCC phase I clinical trial. These studies have a mix of N1 and M1 patients, with various EBRT regimens used:
Dr. Mottet emphasized that the evidence for metastasis directed therapy alone (no ADT) has only one study [1] of 28 patients with bone oligometastases (<= 4) on PSMA PET/CT only. Over a median follow-up of 22 months, the distant progression free survival rate was 45.3% at 1 year and 27% at 2 years. At the recent APCCC 2022 meeting, for the majority of newly diagnosed patients with up to 3 bone metastases on next generation imaging, 61% of the experts would use systemic therapy + local therapy to the primary + metastasis directed therapy, whereas 33% would only use systemic therapy + local therapy to the primary. Additionally, the NCCN guidelines suggest that PSMA-PET/CT or PSMA-PET/MRI can serve as equally effective, if not more effective in front-line imaging for these patients, and that PSMA-11 or F-18 piflufolastat PSMA PET/CT or PET/MRI can be considered for bone and soft tissue (full body) imaging.
Dr. Mottet concluded his presentation discussing that limited bone involvement detected by PSMA PET/CT is associated with palliative treatment with the following take-home messages:
- PSMA positive lesions in the bone (confirmed with coupled CT imaging) is a systemic disease
- Systemic disease is a non-curative situation in most cases
- Systemic therapy is standard of care and added modalities, such as metastasis-directed therapy, should be discussed in the context of clinical trials
Presented by: Nicolas Mottet, MD, PhD, Department of Urology, University Hospital Nord, Saint Etienne, France
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 European Association of Urology (EAU) Annual Hybrid Meeting, Amsterdam, NL, Fri, July 1 – Mon, July 4, 2022.
References:
Related Content:
EAU 2022: Limited Bone Involvement Detected by PSMA PET Only: From Curative to Palliative Treatment? NO


