(UroToday.com) The 37th Annual European Association of Urology Congress held in Amsterdam, the Netherlands between July 1st, and 4th 2022 was host to a session about management of metastatic hormone sensitive prostate cancer (mHSPC). Professor Tarik Esen was tasked with discussing the role of prostate-specific membrane antigen (PSMA)-PET/CT for staging and monitoring of advanced prostate cancer.
Dr. Esen began his presentation by noting that the use of PSMA-PET/CT has been incorporated into the EAU guidelines on primary staging for high-risk localized disease/locally advanced disease: “When using PSMA PET or whole-body MRI to increase sensitivity, be aware of the lack of outcome data of subsequent treatment changes.” (Strong recommendation)
Conventional imaging for primary staging has limited sensitivity. For detection of lymph node involvement, abdominal CT and MRI have limited sensitivities and of 39-42% and specificity of 82%. The same limitations apply to bone scans for metastatic screening. This test is PSA dependent with sensitivities of 2.3% for PSA <10 ng/dL and 16.2% for PSA of 20.0-49.9 ng/dL. PSMA performs much better than bone scan in this setting with sensitivity of 96.2% (versus 73.1% for bone scan) and specificity of 99.1% (versus 84.1% for bone scan).
The proPSMA trial, a prospective, multicenter study of patients with untreated high-risk PCa randomized to 68Ga-PSMA-11 PET/CT or conventional imaging demonstrated that PSMA-PET/CT had 27% greater accuracy than conventional imaging:1
- 92% accuracy for PSMA PET/CT
- 91% for pelvic LN metastases
- 95% for distant metastases
- 65% accuracy for conventional imaging
- 59% for pelvic LN metastases
- 75% for distant metastases
What about the role of PSMA-PET/CT in the detection of LN involvement for pre-operative surgical planning in patients with prostate cancer? A 2022 systematic review of 27 studies by Stabile et al. demonstrated the following performance characteristics:2
- Sensitivity: 58% (95% CI: 50 – 66%)
- Specificity: 95% (95% CI: 93 – 97%)
- PPV: 79% (95% CI: 72 – 85%)
- NPV: 87% (95% CI: 84 – 89%)
- This means that of 100 patients with negative PSMA PET/CT imaging for LN involvement, 87% will have no evidence of pathologic LN involvement following a PLND. As such, 13% of patients would have missed LN involvement if PLND was foregone.
In 2021, Dr. Esen’s group published on their experience with PSMA-PET/CT for primary staging in 96 patients who subsequently underwent a radical prostatectomy with PLND. On a per-patient level, sensitivity and specificity were 53.3% and 98.8%. On a pre-lesion level, sensitivity was 31% and specificity was 98.8%.
In the post-radical prostatectomy biochemical recurrence disease space, there is also strong evidence for the role of PSMA-PET/CT in this setting. Perrera et al. in 2019 demonstrated that PSMA-PET/CT has high positivity even at low PSA values:
- PSA <0.2: 33%
- PSA 0.2-0.49: 45%
PSMA-PET/CT has better diagnostic accuracy compared to:
- 18F-fluciclovine PET/CT (Calais et al. Lancet Oncol. 2019)
- 18F-choline PET/CT (Afshar-Oromieh et al. Eur J Nucl Med Mol Imaging. 2014)
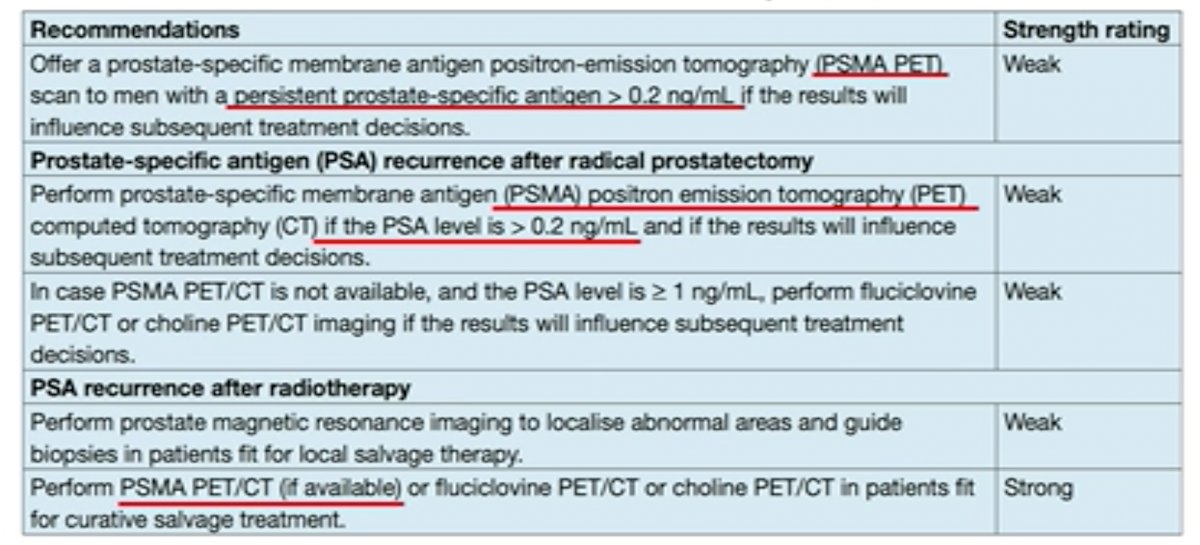
These findings have now been reflected in the most recent EAU guidelines for imaging in patients with biochemical recurrence/PSA persistence:
Now that PSMA-PET/CT has been shown to improve detection of LNs and metastatic sites, Dr. Esen asks:
- Does it change the management plan?
- Does superior detection of metastatic lesions provide better oncological outcomes?
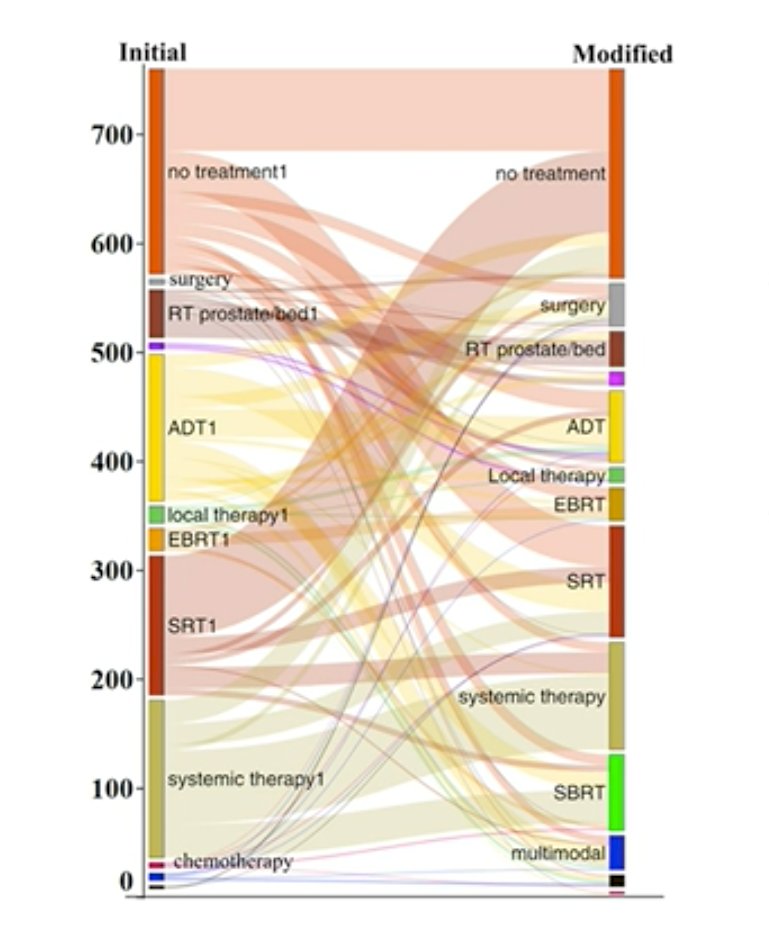
To this end, Dr. Esen presented data from a 2018 Australian prospective multicenter study that evaluated the impact of 68Ga-PSMA-PET/CT on management intent in prostate cancer. A total of 431 patients with prostate cancer from fourAustralian centers had pre- and post-68Ga-PSMA management plans completed. Scans were obtained for primary staging of intermediate- and high-risk disease in 25% of patients and for restaging/biochemical recurrence in 75% of patients. PSMA-PET/CT revealed unsuspected disease:
- Prostate bed: 27%
- Locoregional LN: 39%
- Distant metastatic disease: 16%
These findings led to an overall change in planned management of 51%.
- BCR after surgery/radiotherapy: 62%
- Primary staging: 21%
Diao et al. in 2021 demonstrated that PSMA-PET/CT led to a similar pooled treatment change in 53% of cases (51% in early BCR of PSA 0.2-0.5 ng/dL). Most of these changes were intermodal in nature (42%).
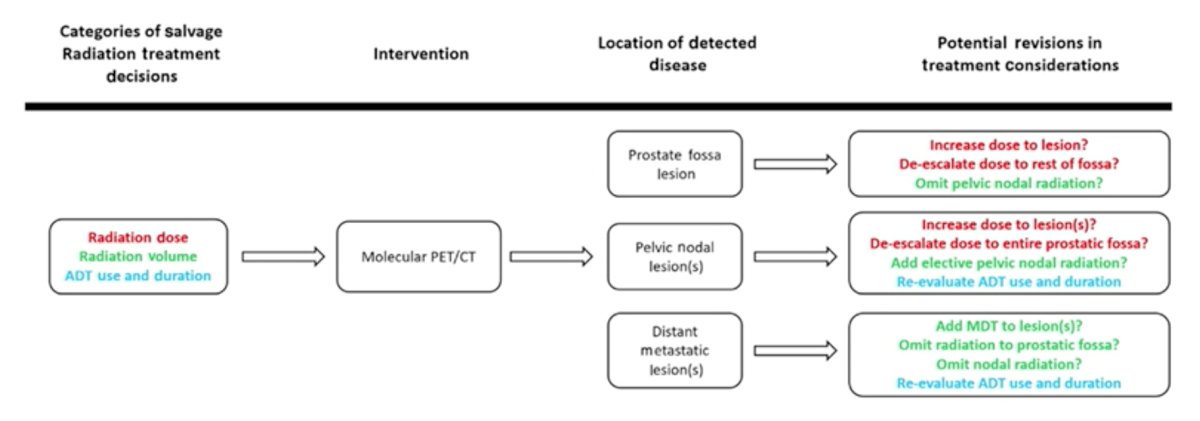
Findings from PSMA-PET/CT have also altered salvage radiotherapy management, in terms of radiation dose, volume, and ADT use/duration., in 77% of patients after 68Ga-11-PSMA-PET/CT.
What about PSMA-PET/CT for treatment monitoring? Currently, there is limited data in this disease space. Following exposure to ADT, there is an initial PSMA upregulation, followed by PSMA expression downregulation after 3 months of ADT. Following exposure to abiraterone/enzalutamide, there appears to be increased PSMA expression and no PSMA flare. There appears to be a correlation between PSMA response and RECIST criteria in patients with mCRPC receiving 3 cycles of docetaxel. However, as demonstrated by Aggarwal et al in Eur Urol Oncol in 2018, PSMA flares without disease progression and discordant results with PSA level have been reported in patients with mCRPC.
In 2021, Fanti et al. proposed the following consensus statements on PSMA-PET/CT response criteria:
- PSMA should only be used if treatment plan is expected to change
- Repeat PSMA is recommended to not be performed earlier than 3 months to avoid the “flare” phenomenon
- PSMA should categorize patients as:
- Non-responders
- Responders (Stable disease/Partial response/Complete response)
- Semi-quantitative evaluation with SUV parametric and volumetric PET measurements are recommended
Imaging findings from PSMA-PET/CT also independently predict outcomes after 177Lu-PSMA therapy. Gafita et al. demonstrated that number of metastatic sites (>=20 versus <20) and tumor SUV) predicted overall survival in treated patients. Patients with higher tumor SUV had associated improved OS (HR: 0.94, p=0.0078), PSA-PFS (HR: 0.92, p=000052), and PSA decline >=50% (HR: 2.88, 95% CI: <0.0001).
Dr. Esen believes that the following questions remain unanswered:
- It is unclear if changes in management after new imaging translate to improved clinical outcomes
- What do we do if conventional imaging is negative, but novel imaging shows metastatic disease:
- Do we abandon standard of care (surgery/radiotherapy?) to avoid unnecessary treatment? (Possible undertreatment?)
- Do we intensify treatment (early systemic treatment, metastasis-directed treatment) to possibly improve outcome? (Morbidity, toxicity, cost?)
Dr. Esen ended his presentation by echoing the following take home messages by Hussain et al. published in JCO in 2021:
- We should move away from a one-size-fits-all approach and accomplish more personalized management. Highly sensitive, accurate, and clinically relevant radiographic assessment of disease is vital.
- Although PET imaging should be considered, patient management should move forward, guided mainly by established principles and existing level 1, evidence-based standard of care.
- One may consider offering additional treatment based on careful consideration of the risks and benefits – and within prospective trials.
Presented by: Professor Tarik Esen, MD, Department of Urology, American Hospital Istanbul, Istanbul, Turkey
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2022 European Association of Urology (EAU) Annual Hybrid Meeting, Amsterdam, NL, Fri, July 1 – Mon, July 4, 2022.
References:
- Hofman MS, et al. A prospective randomized multicentre study of the impact of gallium-68 prostate-specific membrane antigen (PSMA) PET/CT imaging for staging high-risk prostate cancer prior to curative-intent surgery or radiotherapy (proPSMA study): clinical trial protocol. BJU Int. 2018;122(5):783-93.
- Stabile A, et al. Can Negative Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography Avoid the Need for Pelvic Lymph Node Dissection in Newly Diagnosed Prostate Cancer Patients? A Systematic Review and Meta-analysis with Backup Histology as Reference Standard. Eur Urol Oncol. 2022;5(1):1-17.Can Negative Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography Avoid the Need for Pelvic Lymph Node Dissection in Newly Diagnosed Prostate Cancer Patients? A Systematic Review and Meta-analysis with Backup Histology as Reference Standard. Eur Urol Oncol. 2022;5(1):1-17.


