(UroToday.com) The 37th Annual European Association of Urology Congress held in Amsterdam, the Netherlands between July 1st, and 4th 2022 was host to a session about management of metastatic hormone sensitive prostate cancer (mHSPC). Dr. Eugen Jan Karol Axcrona was tasked with discussing future perspectives in the management of metastatic hormone sensitive prostate cancer (mHSPC).
Dr. Axcrona began his presentation by noting that there are approximately 1.5 million incident cases of prostate cancer annually, with ~20% of them metastatic at presentation.

The benefit of adding androgen receptor blockade to ADT has been shown as early in 2004, where a Japanese trial demonstrated that bicalutamide 80 mg in combination with an LHRH agonist is superior to LHRH agonist monotherapy as first-line treatment for advanced prostate cancer (Jpn J Clin Oncol 2004). Early treatment intensification in mHSPC with ADT+ abiraterone doublet therapy in LATITUDE or triplet therapy with ADT + docetaxel + androgen receptor inhibitor (ARI) with either abiraterone (PEACE-1) or darolutamide (ARASENS) has been shown to improve overall survival (OS) and surrogate endpoints such as rPFS or time to castration resistance.1
Dr. Axcrona raised the following questions:
- What is the benefit of adding docetaxel to maximal androgen blockade with a modern ARI? ARASENS and PEACE-1 demonstrated that addition of the ARI to ADT + docetaxel improves outcomes, but what about adding docetaxel to ADT+ARIs?
- What is the benefit of adding local treatment to maximal androgen blockade with a modern ARI? The STAMPEDE arm H trial investigated local treatment in patients treated for the most part with ADT alone (18% received early docetaxel)
- What is the benefit of metastatic targeted therapy for patients with oligometastatic disease? Currently, evidence in favor of this treatment approach is limited to small phase II trials with limited follow up.
- Is there a group of patients for whom treatment (or part of the treatment) can held after a while? As of today, the only group eligible for this potentially is the PSA <0.2 ng/ml group, but Dr. Axcrona believes we need to do better.
The keys remain: imaging, genomics, and biomarkers.
“The train has left for the use of PSMA-PET/CT” was a phrase commonly used at the latest APCCC meeting in Lugano. This implies, in part, that current trials in this disease space are not able to accommodate PSMA-PET/CT usage in their current protocols. Dr. Axcrona’s personal view is that PSMA-PET/CT should be incorporated in future studies in mHSPC when high volume disease is not detected by conventional imaging. If conventional imaging identifies high volume disease patients, then additional metastatic disease findings with PSMA-PET/CT are of no additive benefit. In addition to PSMA PET/CT’s ability to properly secure disease volume in relation to various treatments, PSMA-PET/CT can act as a biomarker, particularly with regards to SUV signal and its utility in predicting response to Lutetium-based theranostics therapy.
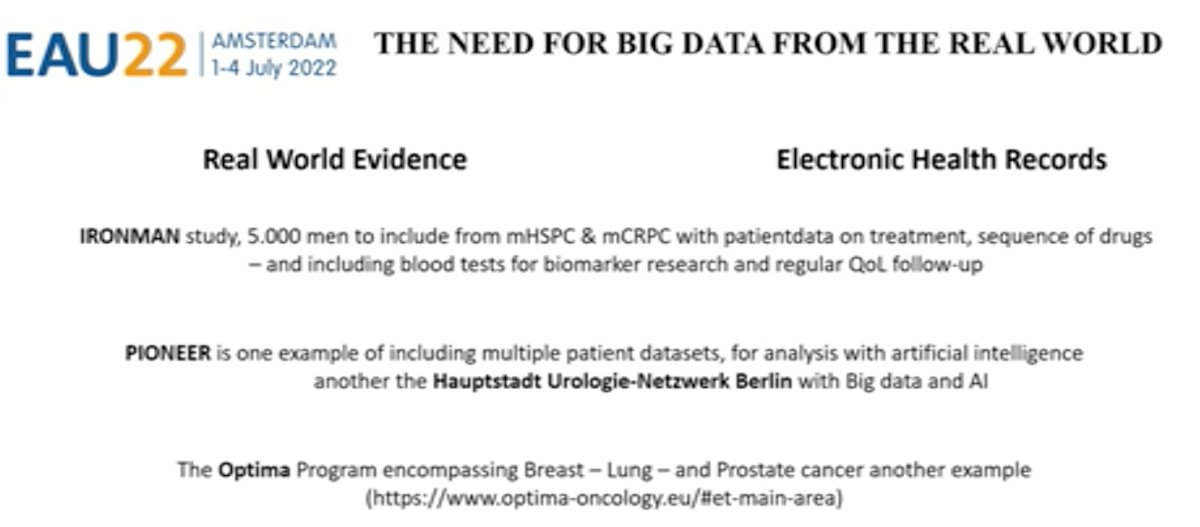
The importance of biomarkers moving forward cannot be overstated. In addition to potential imaging-based biomarkers, genomic biomarkers, including DDR gene mutations, are critical for evolving the field of precision medicine. One concern with the genomic approach is the genomic heterogeneity of both the primary prostate cancer and distant metastatic lesions. Indeed, the variability among unifocal prostate cancer cases is ~20-30%, compared to 70-80% for multifocal cases. In Dr. Axcrona’s opinion, there remains a need for “big data” from the “real world” to supplement the genomic data available from clinical trials.
Dr. Axcrona concluded his presentation with his personal take on the future perspective of mHSPC:

Presented by: Dr. Eugen Jan Karol Axcrona, MD, PhD, Department of Urology, Akershus University Hospital, Lorenskog, Norway
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2022 European Association of Urology (EAU) Annual Hybrid Meeting, Amsterdam, NL, Fri, July 1 – Mon, July 4, 2022.
References:


