(UroToday.com) The 2023 European Association of Urology (EAU) annual congress held in Milan, Italy between March 10th and 13th, 2023 was host to a session addressing precision medicine in patients with metastatic castrate-resistant prostate cancer (mCRPC). Dr. Elena Castro delivered a state-of-the-art lecture discussing mCRPC patient-related factors that guide treatment decisions.
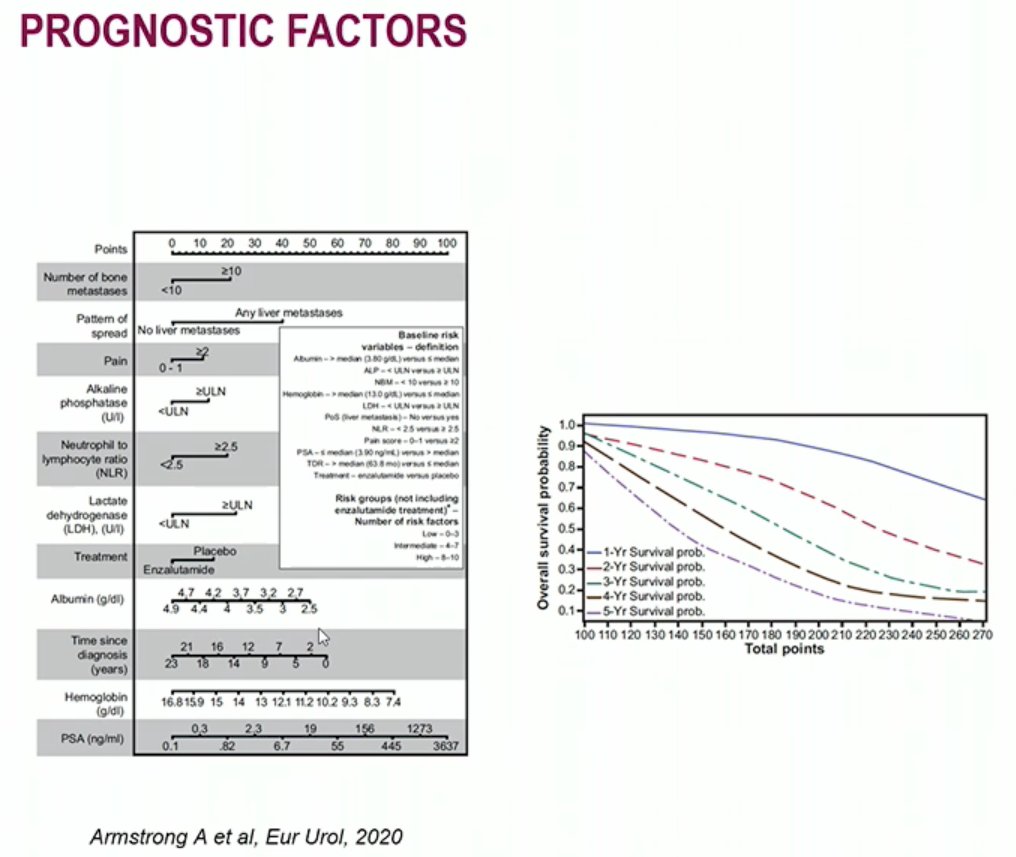
There are numerous well-established clinical prognostic factors in mCRPC among which these include:
- Time to progression on previous therapies
- Number of bone metastases
- PSA kinetics
- ECOG performance status
- Presence of pain and use of opiates
- Hemoglobin
- LDH
- Albumin
- Alkaline phosphatase
- Neutrophil to lymphocyte ration (NLR)
Several biomarkers in this disease space have prognostic value, such as AR aberrations, TP53 mutations, RB1 loss, and CDK12 mutations. However, none of these genetic biomarker mutations have “direct” actionable treatment targets as of yet and such alterations have a modest impact on clinical practice.

Dr. Castro then provided a nuanced approach to the selection of mCRPC therapy based on patient-level factors. As demonstrated in the figure below, factors include mobility, cognition, mood, social vulnerability, disease state, nutrition, energy, and function levels.

One often under-valued patient factor in treatment selection remains patient frailty (medical, social, and functional deficits). Frailty is a complex, multidimensional state of diminished physiological reserve that results in decreased resiliency and adaptive capacity and increased vulnerability to stressors. Frail patients are at increased risk of postoperative complications, chemotherapy intolerance, disease progression, and death.

We must also not be fooled by a patient’s chronological age, but, instead, should focus on biological age. As demonstrated in the bar graph below, there are wide variations in the life expectancy among elderly patients, particularly in the “younger” cohort of patients in their 70s, whereby life expectancy can vary between 18 and 6.7 years in those aged 70 years.

What are some tools that we can use in clinical practice to assess frailty in elderly patients? The geriatric screening with G8 tool and mini-COGTM, with simplified geriatric evaluation if the G8 is 14 or less:

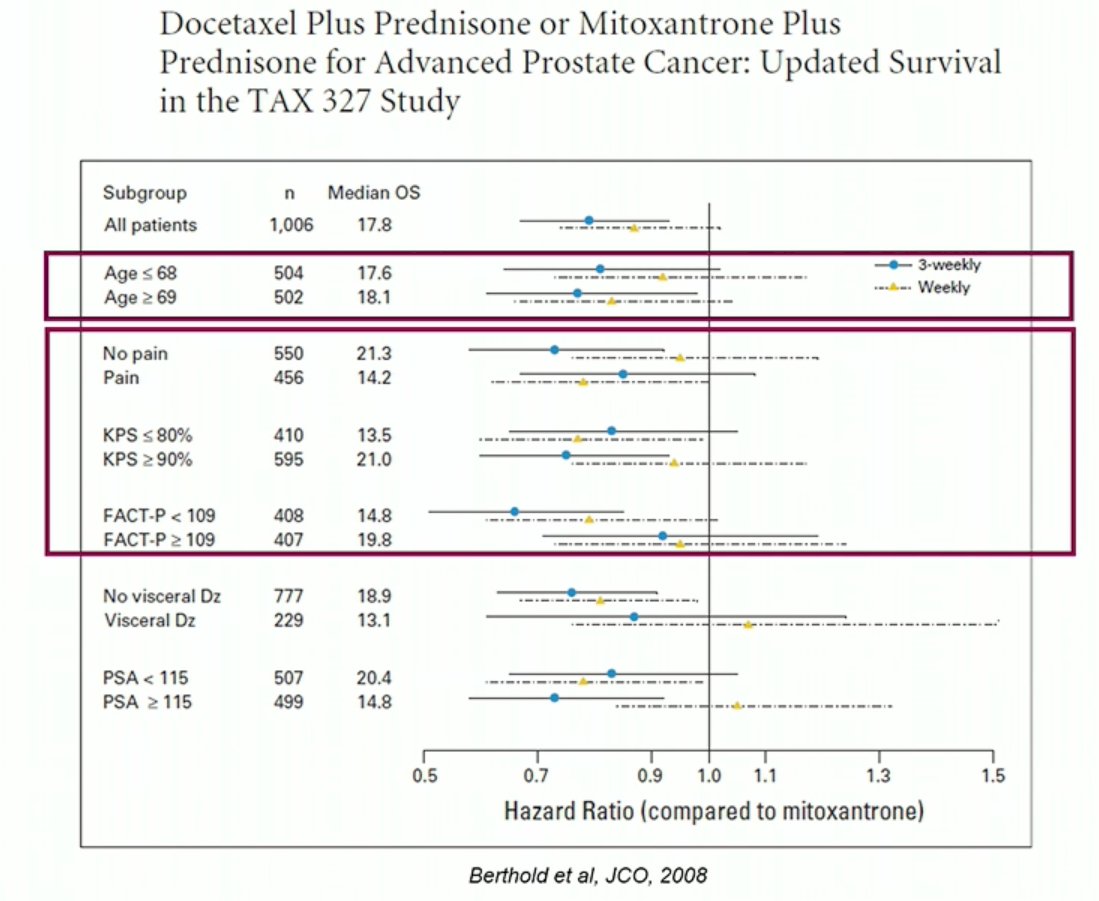
There is a common misconception that taxane chemotherapy should be avoided in elderly patients. Analysis from the TAX-327 study has demonstrated that elderly patients ages 69 and above derive a significant benefit from taxane chemotherapy in the mCRPC setting, with an even more pronounced effect estimate compared to younger patients.1
One option available to reduce the toxicity profile and incidence of adverse events is the use of a dose-reduced 2-weekly versus 3-weekly docetaxel regimen, which have equivalent oncologic efficacy.

Cabazitaxel has also been used in elderly patients, however, compared to docetaxel, has a worse toxicity/AE profile, particularly with regards to febrile neutropenia. However, prophylactic measures such as the use of C20 and G-CSF primary prophylaxis may reduce this toxicity profile.
While a lot of the focus has been on the toxicity of taxanes in elderly patients, novel hormonal agents such as abiraterone also have significant adverse events in elderly, chemonaïve patients, particularly with regards to fluid retention. Dr. Castro recommended that such patients receive a pre-treatment echocardiogram to risk stratify them in the pre-treatment setting.

This is also applicable to other NHA agents such as enzalutamide, which has significant drug-drug interactions particularly in poly-medicated elderly patients. Enzalutamide is also associated with significant fatigue and falls as side effects.

With the emergence of theranostics such as Lu-PSMA with anticipated use in elderly patients, we must keep in mind that these agents have similar efficacy in elderly patients, at the cost of more frequent fatigue.

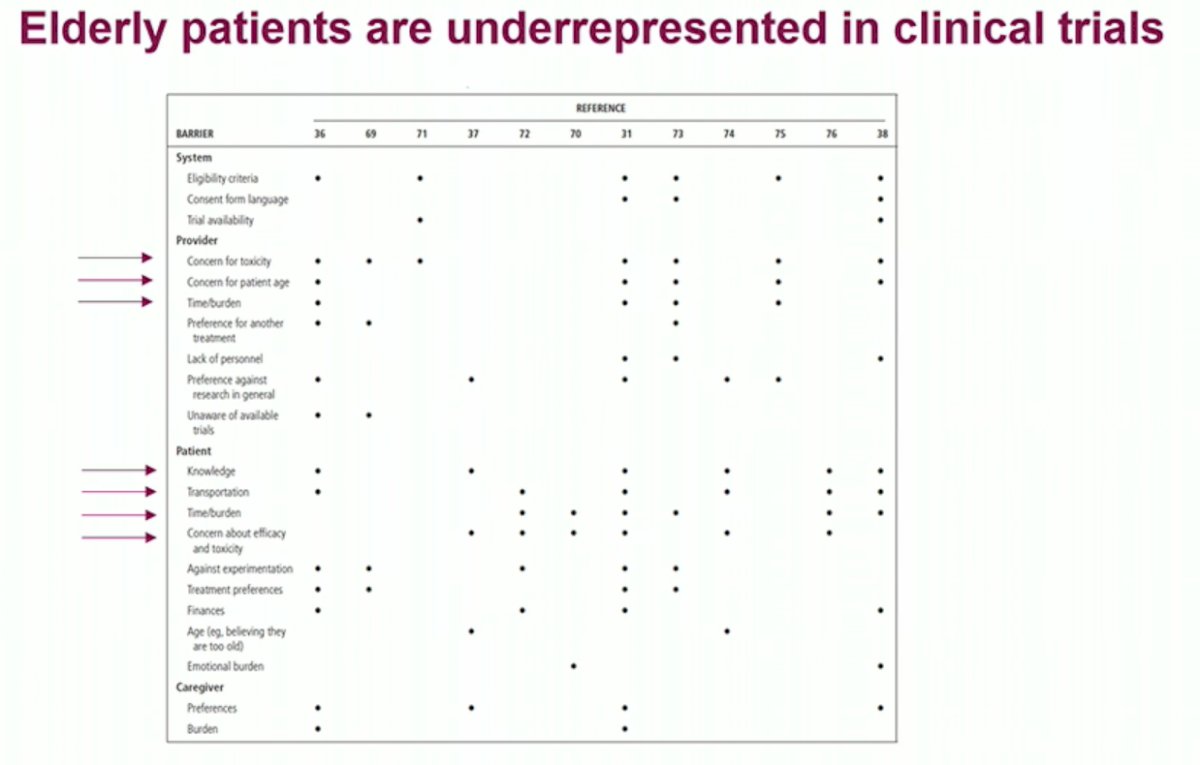
One historic issue that needs to be addressed in future trials is the significant underrepresentation of elderly patients in clinical trials. Clinical trials select for “healthier” patients who are classically younger, have better performance status, and thus are more likely to benefit from and tolerate the study drug.
Dr. Castro concluded her presentation by highlighting the patient-related factors that should guide systemic treatment decisions:
- Prognostic variables and biomarkers
- Comorbidities, life expectancy
- Eligibility for clinical trials
- Patient’s preferences
- Drug-drug interactions
- Expected toxicities
- Predictive biomarkers
- Previous therapies
- Availability, reimbursement, financial toxicity
Presented by: Dr. Elena Castro, MD, MS, PhD, Medical Oncology, Hospital Universitario, Madrid, Spain
Written by: Rashid K. Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2023 European Association of Urology (EAU) Annual Meeting, Milan, IT, Fri, Mar 10 – Mon, Mar 13, 2023.
References:- Berthold et al. Docetaxel Plus Prednisone or Mitoxantrone Plus Prednisone for Advanced Prostate Cancer: Updated Survival in the TAX 327 Study. Journal of Clinical Oncology, 2008. 242-245.


