The first paper discussed was the open-label randomized, phase 3 non-inferiority trial comparing robotic radical cystectomy (RARC) to open radical cystectomy (ORC), published in Lancet in 2018. This was a multicenter study including 15 centers in the US. The involved surgeons were required to have performed at least ten radical cystectomies before study initiation. All the diversions done in the robotic group were extracorporeal, and patients were randomized 1:1. The primary endpoint was progression-free survival at two years, and the non-inferiority margin that was chosen was 15%. The secondary endpoints included blood loss, the proportion of patients requiring a blood transfusion, surgical margin status, number of lymph nodes resected, operating time, length of hospital stay, surgical complications at 90 days, change in health-related quality of life, and outcomes at 3 and six months postoperatively.
The study demonstrated that RARC was non-inferior to ORC with a 2-year progression-free survival of 72.3% and 71.6% in the RARC and ORC groups, respectively (Figure 1).
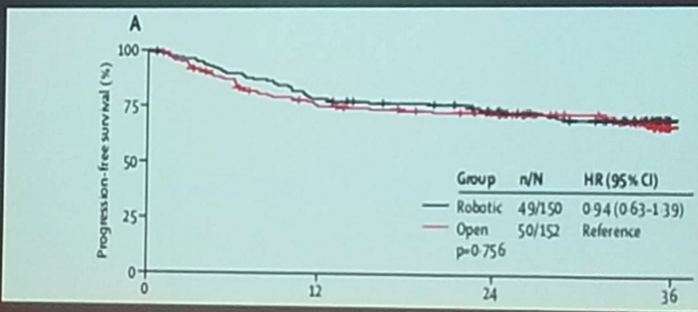
Figure 1 – Progression-free survival in robotic radical cystectomy vs. open radical cystectomy:
Additionally, local and distant recurrence rates were similar among the groups (3% vs. 4% local recurrence, and 23% vs. 22% distant recurrence rates in RARC and ORC, respectively). There was a 0% rate of port site metastasis in the RARC group.
To date, this is the best level of evidence that exists regarding the equivalence of RARC to ORC, although some limitations need to be mentioned. These include the fact that no intracorporeal diversions were performed in the RARC group. Additionally, no clear ERAS protocol and clinical pathways were used. Lastly, the surgical experience of the surgeons involved in the RARC study was perhaps a limitation.
Another discussed paper looked at the outcomes of 1094 intracorporeal diversions after RARC in 26 institutions and its comparison to extracorporeal diversion. The study spanned a period between 2005 and 2015.2 Intracorporeal urinary diversion use increased from 9% of all urinary diversions in 2005 to 97% in 2015. Complications after this procedure decreased significantly with time. A total of 80% of the intracorporeal diversions were an ileal conduit, and approximately 16% were neobladders. In this study, prior abdominal surgery was the only significant predictor of major complications in RARC. No differences in recurrence-free survival and disease-specific survival were evident between extracorporeal and intracorporeal diversions.
Dr. Tyritzis moved on to discuss the impact of packed red blood cells and fresh frozen plasma given during radical cystectomy on cancer-related outcomes and survival.3 The predictive factors for transfusions included neoadjuvant chemotherapy, preoperative anemia, older age, and ASA score >3. Receipt of blood products was associated with a higher 90 d mortality, inferior 5-year recurrence-free survival, 5-year cancer-specific survival, and 5-year overall survival. In multivariable analysis, blood transfusion was predictive for all-cause mortality [HR 1.610; p<0.001] and cancer-specific mortality (HR 1.467; p=0.010).
Lastly, Dr. Tyritzis discussed a study analyzing the cost-effectiveness of RARC vs. ORC.4 In summary; the study demonstrated that there is a 23% probability for cost-effectiveness of RARC when it achieves:
- Shortened operating times (threshold of 175 minutes)
- Length of stay (threshold of 4 days)
- Cost reduction in RARC equipment (threshold of 281$)
Dr. Tyritzis summarized his talk stating that RARC is shown to be equal in all aspects to ORC, both in oncological and functional outcomes. Dr. Tyritzis believes that use of RARC will continue to grow in the upcoming future.
Presented by: Stavros I. Tyritzis, Karolinska Institutet, Sweden, and Athens Medical Center
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the EAU Robotic Urology Section (ERUS) Meeting - September 5 - 7, 2018 - Marseille, France
References:
1.Parekh DJ, Reis IM, Castle EP, et al. Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): an open-label, randomised, phase 3, non-inferiority trial. Lancet (London, England) 2018; 391(10139): 2525-36.
2.Hussein AA, May PR, Jing Z, et al. Outcomes of Intracorporeal Urinary Diversion after Robot-Assisted Radical Cystectomy: Results from the International Robotic Cystectomy Consortium. The Journal of urology 2018; 199(5): 1302-11.
3.Furrer MA, Fellmann A, Schneider MP, et al. Impact of Packed Red Blood Cells and Fresh Frozen Plasma Given During Radical Cystectomy and Urinary Diversion on Cancer-related Outcome and Survival: An Observational Cohort Study. European urology focus 2017.
4.Michels CTJ, Wijburg CJ, Leijte E, et al. A cost-effectiveness modeling study of robot-assisted (RARC) versus open radical cystectomy (ORC) for bladder cancer to inform future research. European urology focus 2018.


