The goals of PLND include:
- Accurate staging – for prognostication and to guide adjuvant chemotherapy
- Therapeutic benefit - survival and local relapse
- Minimize morbidity – low complication rate
The PLNDy templates can be divided into several zones (Figure 1). The median number of lymph nodes removed from each location1 is demonstrated in figure 2. Almost all lymph nodes are found up to the level of the ureter crossing the common iliac vessels (Figure 3). There are different templates for PLND, including limited, extended and super-extended (Figure 4).
Figure 1 – Lymphadenectomy zones:
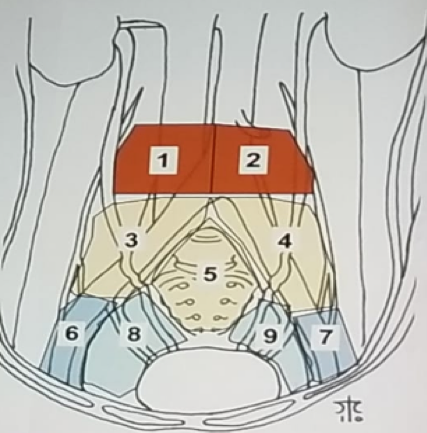
Figure 2 – Median number of lymph nodes removed from each zone:
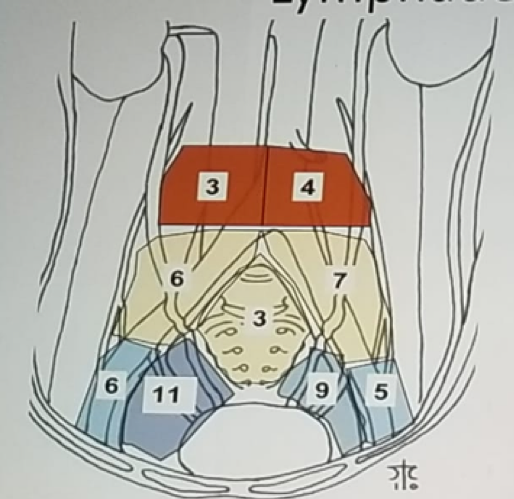
Figure 3 – Locations of positive lymph nodes:

Figure 4 – Pelvic lymphadenectomy templates:
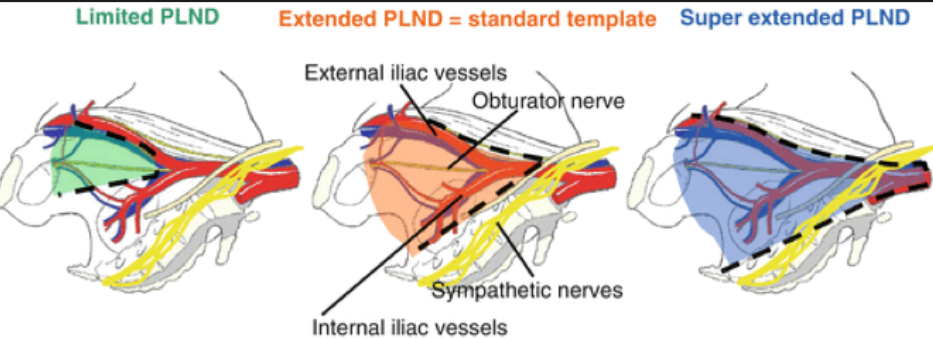
The outcomes of PLND are predicted by pathological T stage, the number of positive lymph nodes removed, the density of positive lymph nodes, their location, the extent of PLND performed and the nodal yield. When comparing PLND to no PLND, studies have shown that no PLND yields increased mortality2, with 5-year cancer-specific mortality of 65% for PLND vs. 54% for no PLND3. A systematic review of 7 studies demonstrated that any PLND is better than no PLND, and extended PLND is better than standard PLND, while no benefit was seen from super extended PLND4.
Interestingly, PLND has even shown benefit in patients with no lymph node involvement. A published study demonstrated that a cutoff of 16 nodes (all negative) yielded a higher cancer-specific survival of 83% vs. 72% for a lower number of removed nodes5. Furthermore, the cancer-specific death two years post-cystectomy was higher among patients with a lower number of negative lymph nodes removed (16% for ten nodes removed vs. 5.5% for 30 nodes removed)6.
Extended PLND has been shown to be better than non-extended PLND in a meta-analysis of 6 studies, including almost 3000 patients. The recurrence-free survival was better for patients with pathological stage T3-T4 and patients with involved and uninvolved lymph nodes7. However, when comparing extended vs. super-extended PLND no improved outcomes were evident.
Dr. Moon summarized his talk by stating that there are currently two randomized controlled trials assessing the impact of PLND in RC (Figure 5). The key take-home messages should be that there is a substantial amount of evidence demonstrating the oncological benefit of PLND for both node-positive and node-negative disease. Prognostic information from resected nodes can help us guide management. Extended PLND provides optimal recurrence-free survival, and cancer-specific survival, while no additional benefit can be seen with super-extended PLND. To date, until results of level 1 evidence are published, recommendations for the optimal PLND template are limited.
Figure 5 – Level 1 evidence for the role of pelvic lymphadenectomy in radical cystectomy:

Presented by: D. Moon, Melbourne, Australia
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the EAU Robotic Urology Section (ERUS) Meeting - September 5 - 7, 2018 - Marseille, France
References:
- Dorin RP, Daneshmand S, Eisenberg MS, et al. Lymph node dissection technique is more important than lymph node count in identifying nodal metastases in radical cystectomy patients: a comparative mapping study. European Urology 2011; 60(5): 946-52.
- Konety BR, Joslyn SA, O'Donnell MA. The extent of pelvic lymphadenectomy and its impact on outcome in patients diagnosed with bladder cancer: analysis of data from the Surveillance, Epidemiology, and End Results Program database. The Journal of Urology 2003; 169(3): 946-50.
- Larcher A, Sun M, Schiffmann J, et al. Differential effect on survival of pelvic lymph node dissection at radical cystectomy for muscle-invasive bladder cancer. European journal of surgical oncology: the journal of the European Society of Surgical Oncology and the British Association of Surgical Oncology 2015; 41(3): 353-60.
- Bruins HM, Veskimae E, Hernandez V, et al. The impact of the extent of lymphadenectomy on oncologic outcomes in patients undergoing radical cystectomy for bladder cancer: a systematic review. European Urology 2014; 66(6): 1065-77.
- May M, Herrmann E, Bolenz C, et al. Association between the number of dissected lymph nodes during pelvic lymphadenectomy and cancer-specific survival in patients with lymph node-negative urothelial carcinoma of the bladder undergoing radical cystectomy. Annals of surgical oncology 2011; 18(7): 2018-25.
- Crozier J, Papa N, Perera M, et al. Lymph node yield in node-negative patients predicts cancer-specific survival following radical cystectomy for transitional cell carcinoma. Investigative and clinical urology 2017; 58(6): 416-22.
- Bi L, Huang H, Fan X, et al. Extended vs non-extended pelvic lymph node dissection and their influence on recurrence-free survival in patients undergoing radical cystectomy for bladder cancer: a systematic review and meta-analysis of comparative studies. BJU international 2014; 113(5b): E39-48.


