The costs associated with robotic surgery include the initial investment in the robotic system, the maintenance, instruments, additional required equipment, and low operating theater efficiency (1-2 cases per 8-hour shift). However, robotic surgery can also bring money to the hospital, when it is a high-volume center, with high operating theater efficiency (3-4 cases per 8-hour shift), when instrument are used in a smart, economical way, when eventually, other robotic companies enter the market, and if the patient get involved in the payment for their procedure.

Table 1- Reimbursement per prostatectomy in different countries:
In the Martini Klinik, in Hamburg, Germany, where Dr. Haese works, approximately 2500 prostatectomies are performed per year. This is an academic institution with private and general health care patients. The reimbursement for the patients is DRG based, and the center aims to be a profitable institution. They have developed an economic plan to save as much money as possible. An example of this is making a “reduced” instrument protocol, which still enables to operate normally, but with saving 1127 Euros per case thorough economic use of instruments and disposables. Multiplying this amount per 1150 RALPs done per year in this center, this translates to total savings of 1.3 million Euros.
Another example is avoiding the purchase of various accessories for robotic surgery, which according to Dr. Haese, are not required. Additionally, the hospital mandates a target incision time of 07:45 AM, so that more cases can be performed each day. This is made possible because patients are admitted the previous night, anesthesia team starts to work at 6:45 AM, only elective surgeries are performed, and there is a no cancellation policy – all cases get done, regardless of finishing time.
Another efficient change was the architecture of the operating theaters. They are built in a way that intubation, the actual surgery, and extubation, occur at different adjacent rooms, enabling the turnover time to be less than 45 minutes between each case (Figure 1).
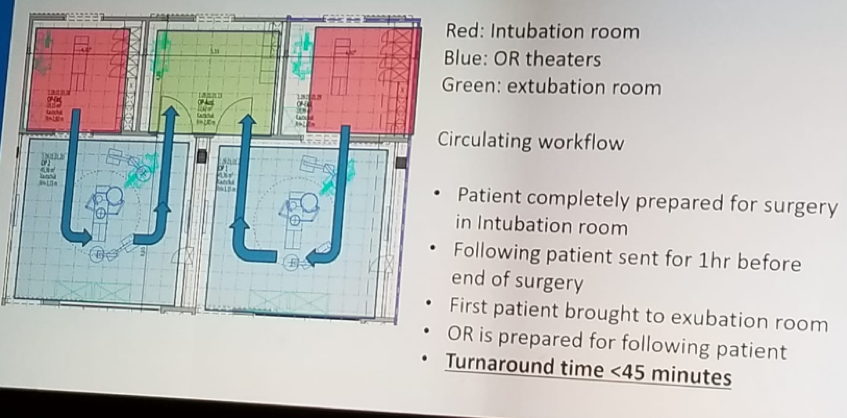
Figure 1 – Efficient operating theater architecture:
Dr. Haese summarized his talk by reiterating that we have no impact on the cost of the initial robotic system, the introduction of newer robots to lower the price, and the reimbursement amount per case. In contrast, we may partially affect the way we subsidize robotics as a profitable procedure, but this might not work out. Most importantly, what we can do is involve the patient in some of the costs, and reduce the cost by economical use of instruments and disposables, by reduction of hospital stay, increased caseload, and operating theater efficiency.
Presented by: A. Haese, Hamburg, Germany
Written by: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, Twitter:@GoldbergHanan at the EAU Robotic Urology Section (ERUS) Meeting - September 5 - 7, 2018 - Marseille, France


