(UroToday.com) The 2022 International Kidney Cancer Symposium (IKCS) European Annual meeting included a session on surgical approaches to kidney cancer and a presentation by Dr. Umberto Capitanio discussing risk classification of renal tumors and how to optimize the future of TMN classification. International guidelines suggest the use of integrated prognostic systems to assess oncologic outcomes at diagnosis or before/after treatment. There are many risk classification scores available, but not many externally validated in recent cohorts. The most frequent covariates used are TNM, grade, and tumor necrosis and/or sarcomatoid features, as well as symptoms, age, and ECOG performance status. Dr. Capitanio notes that treatment decisions and, potentially, outcomes are dramatically influenced by risk classification and its characteristics. This is dependent on: (i) quality and methodology in the original development, (ii) validation and applicability, and (iii) choice by the clinician (which classification scheme is picked). An example of the heterogeneity using EAU risk classification is as follows:
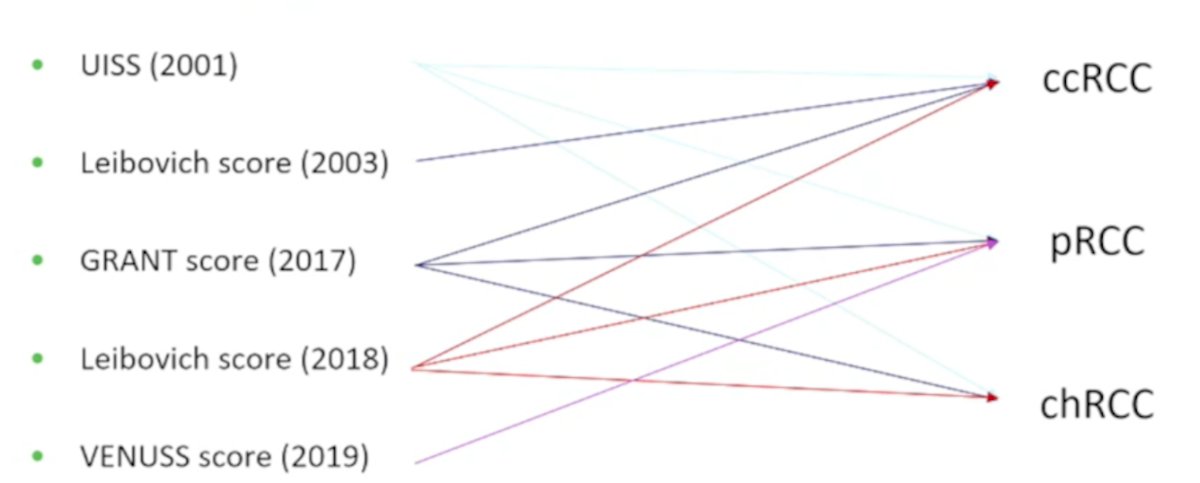
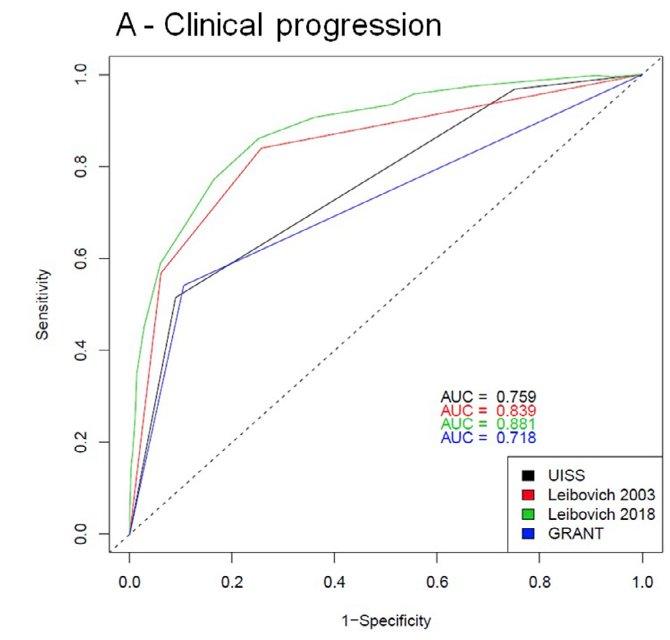
In work from Dr. Capitanio’s group,1 for clear-cell RCC, Leibovich 2018 resulted in the most accurate model for predicting clinical progression (88.1%) and cancer-specific mortality (86.8%). Conversely, VENUSS or UISS prognostic models predicting oncologic outcomes represented the most accurate in papillary (88.7% and 84.8%) or chromophobe (87.8% and 89.1%) RCC, respectively. As follows is the Sankey diagram and ROC curve (for clinical progression) for clear cell RCC:

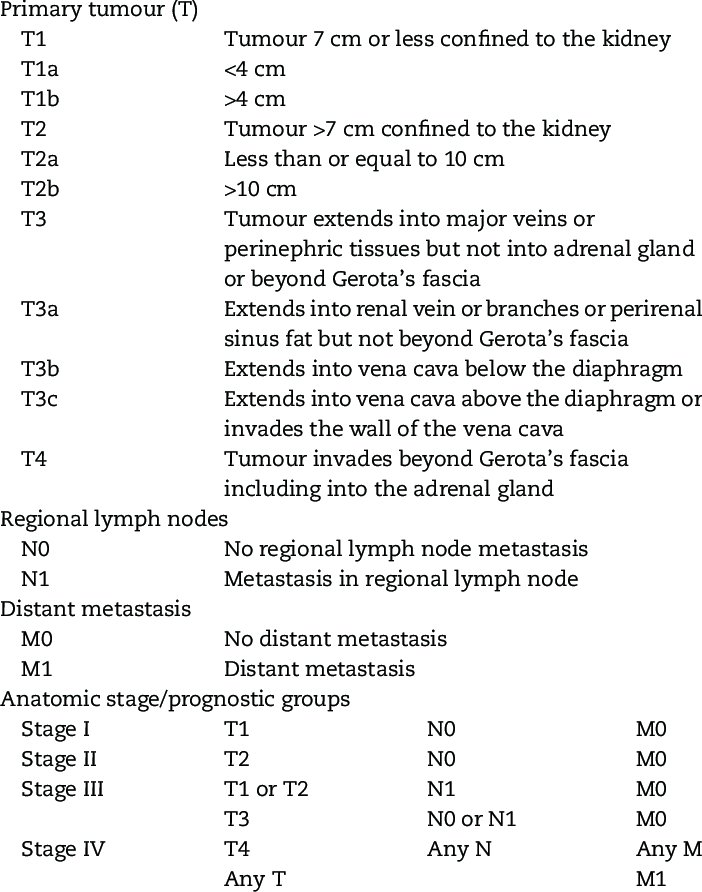
Staging is the single most informative piece of information for risk classification, and currently, the TNM staging (UICC/AJCC) is the most universally accepted staging system. It is simple, convenient, concise, and reproducible. Since its first publication in 1977, UICC/AJCC has undergone changes and as of April 1st, 2018 its 8th edition is used (with the 9th edition coming soon):
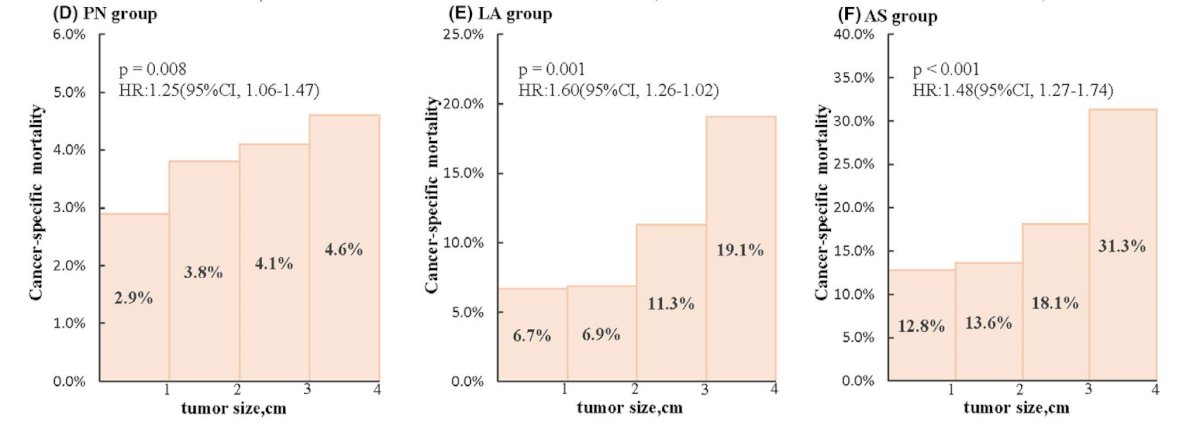
Dr. Capitanio emphasized that in order to optimize the future TNM classification system, we need (i) a critical definition of T1 (= SRM = non-surgical options), and (ii) to decide if it is necessary to size stratify T2 since this has been questioned in the past. Tang et al. [2] recently published a study investigating whether tumor growth in patients with SRMs leads to tumor progression. Among 16,070 patients in the SEER database (2004-2017), four tumor size categories were delineated (≤1, >1– 2, >2–3, and >3–4 cm in diameter). Tumors were subsequently substaged based on diameter: T1aA (≤2 cm) and T1aB (>2– 4 cm), noting that all-cause and cancer-specific mortality were significantly higher in T1aB tumors than T1aA tumors in each group:
With respect to high T stage tumors, Dr. Capitanio notes that renal sinus fat invasion may carry a worse prognosis than perinephric fat invasion, but is nevertheless included in the same pT3a stage group. He also notes that sub T-stage (pT2b, pT3a, pT3c, and pT4) often overlap. Furthermore, when assessing N-stage, Dr. Capitanio notes that we need a critical definition of N1, given that N1 may mean this is locally advanced disease and should be treated surgically versus N1 which is metastatic and patients should receive first-line medical therapy. We also need a clear definition of oligometastatic (which may have implications based on data from CARMENA and SURTIME), perhaps delineating metastatic disease by M1a vs M1b vs M1c.
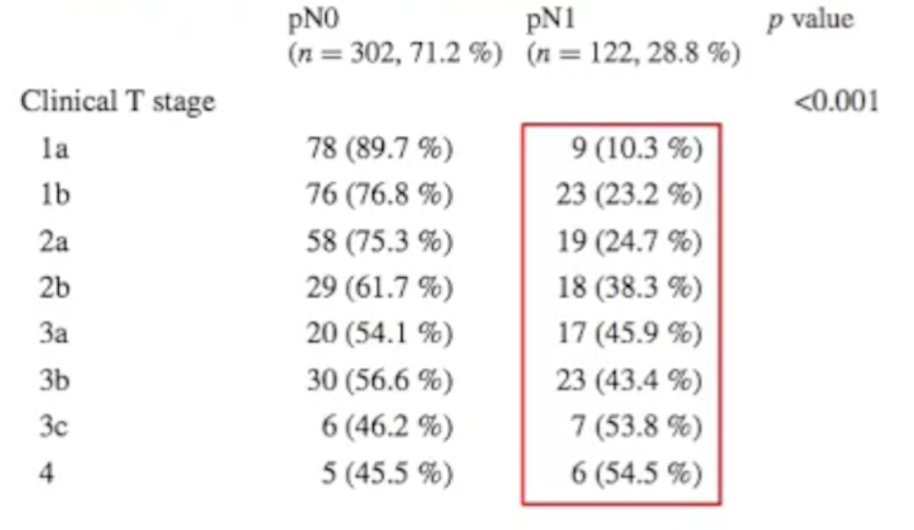
Work from Dr. Capitanio’s group published in 2016 [3] assessed which factors are related to a concordance between clinical suspicion and pathological confirmation of lymph node invasion (LNI). Among 2,954 patients that underwent either partial or radical nephrectomy at San Raffaele, preoperative axial CT scans revealed 424 (14.4 %) patients showing at least one enlarged lymph node suspected of LNI (cN1). All lymphadenopathies were removed at surgery, and LNI was pathologically confirmed (pN1) in 122 patients (28.8 %). Dr. Capitanio notes that there was an increasing gradient with increasing T-stage for the likelihood of pN1 disease:
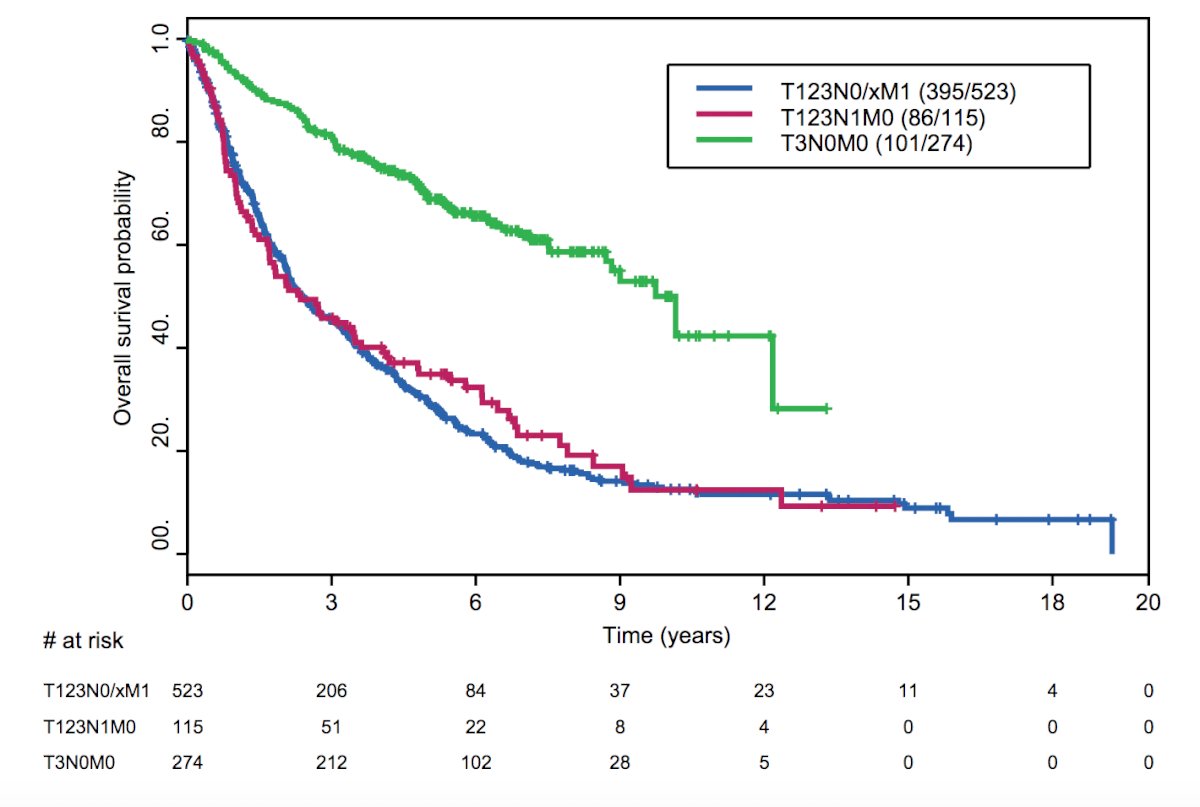
To further clarify TNM staging in locoregional disease, Yu et al. [4] compared the survival outcomes of patients with stage III, node-positive disease (pT123 N1 M0), and patients with stage III, node-negative disease (pT3 N0 M0). Among 4,652 patients undergoing surgery at MD Anderson Cancer Center, 115 patients had pT123 N1 M0 disease, 274 patients had pT3 N0 M0 disease, and 523 patients had pT123 N0/x M1 disease that was included. This study found that median overall survival and cancer-specific survival times were significantly better for pT3 N0 M0 patients than pT123 N1 M0 patients (overall survival 10.2 vs 2.4 years, p < 0.0001; cancer-specific survival times not reached vs 2.8 years, p < 0.0001). Furthermore, similar median overall survival and cancer-specific survival times were noted for pT123 N1 M0 and pT123 N0/x M1 patients (overall survival 2.4 vs 2.4 years; p = 0.62; cancer-specific survival times 2.8 vs 2.4 years; p = 0.10). As follows is the Kaplan-Meier curve for overall survival based on the aforementioned stratification:
Dr. Capitanio concluded his presentation by discussing risk classification of renal tumors and how to optimize the future of TMN classification with the following take-home messages:
- Risk classification in RCC is critical for clinical decision making and patients’ outcomes
- TNM will continue to be a key backbone for risk classification (9th edition is coming)
- Some uncertainties remain (subT1a, T2, T3, N1ab vs M1abc)
- With the rapid expansion of our understanding regarding tumor biology, even more important changes are expected in the future
Presented by: Umberto Capitanio, MD, San Raffaele Scientific Institute, Milan, Italy
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 International Kidney Cancer Symposium (IKCS) Europe Annual Hybrid Meeting, Antwerp, Belgium, Fri, Apr 22 – Sun, Apr 24, 2022.
References:- Rosiello G, Larcher A, Fallara G, et al. Head-to-head comparison of all the prognostic models recommended by the European Association of Urology Guidelines to predict oncologic outcomes in patients with renal cell carcinoma. Urol Oncol. 2022 Feb 6;S1078-1439(21):00558-5.
- Tang Y, Liu F, Mao X, et al. The impact of tumor size on survival of patients with small renal masses: A population-based study. Cancer Med. 2022 Mar 1 [Epub ahead of print].
- Capitanio U, Deho F, Dell’Oglio P, et al. Lymphadenopathies in patients with renal cell carcinoma: Clinical and pathological predictors of pathologically confirmed lymph node invasion. World J Urol. 2016 Aug;34(8):1139-1145.
- Yu K-J, Keskin SK, Meissner MA, et al. Renal cell carcinoma and pathologic nodal disease: Implications for American Joint Committee on Cancer Staging. Cancer. 2018 Oct 15;124(20):4023-4031.


