The first case was a 72-year-old man with a family history of prostate cancer (brother, currently on active surveillance), with a BMI of 22 kg/m2, a non-smoker/non-alcohol user, with a medical history of ischemic heart disease (angioplasty and stent in 2008 and 2010), hypertension, and peptic ulcer disease. His surgical history was significant for an appendectomy and his urologic history included three previous prostate biopsies (2004 and 2006 – negative; 2011 HGPIN). His last PSA was 6.6 ng/mL and his prior transrectal ultrasound (TRUS) ultrasound demonstrated a 49 cc prostate, including a 28 cc of adenoma. His International Prostate Symptom Score (IPSS) was 25 and his IIEF-25 score was 16, a PHI score was 52, his DRE was negative, and a multiparametric MRI (mpMRI) showed a 9mm PI-RADS 3 lesion at the right lateral margin. A subsequent fusion biopsy plus systematic biopsy showed no cancer in the systematic biopsy, but among four targeted cores, there was one core positive for Gleason 3+4 prostate cancer, showing poorly formed glands, 30% core positive and percent pattern 4 of 22%. Following the biopsy, the patient was included in an active surveillance program and subsequent follow-up a year later demonstrated a PSA of 7.9 ng/mL, a negative DRE and an MRI redemonstrating the 9mm PI-RADS 3 lesion at the right lateral margin. He then underwent another fusion biopsy that showed 5/12 cores from the systematic biopsy with Gleason 3+3 disease (right side), and 3/4 targeted cores positive for Gleason 3+4 disease with poorly formed glands. Both CT scan and bone scan were negative for metastatic disease. The patient then opted for a robotic-assisted radical prostatectomy, pathology demonstrating Gleason 4+3, pT3aN0R0. His first post-operative prostate-specific antigen (PSA) was undetectable and he is currently using no pads for incontinence and he does not have erectile function. Dr. Fossati notes that on the positive side, this patient had 16 months of time from diagnosis to local treatment for his prostate cancer, however, given his pT3a Gleason 4+3 pathological disease he may be at increased risk for recurrence.
The second case included a 69-year-old male with a family history of prostate cancer (father, treated with a radical prostatectomy), with a BMI of 24 kg/m2, a non-smoker/non-alcohol user, and a medical history significant for hypertension and hypercholesterolemia. His surgical history was significant for bilateral inguinal hernioplasty, and his urologic history included a PSA of 5.5 ng/mL, TRUS size prostate of 49 cc, an IPSS of 25 and IIEF of 18. A prostate biopsy at an outside institution demonstrated 1/12 cores positive for right-sided Gleason 3+3 prostate adenocarcinoma. Upon pathology review at Dr. Fossati’s institution, this was read as Gleason 3+4, with poorly formed glands, percent core positive of 10%, and percent pattern 4 of 12%. At this point he was enrolled in an active surveillance program. A follow-up PSA six months later demonstrated a PSA of 5.0 ng/mL, negative DRE and a subsequent six-month visit demonstrated a PSA of 5.9 ng/mL, with an MRI suggestive of 12 mm PI-RADS 3 lesion in the right transition zone. A fusion biopsy thereafter was negative for prostate cancer. Dr. Fossati notes that on the positive side, this patient is free from local treatment to the prostate, however, there is a questionable risk of missed disease on fusion biopsy.
Dr. Mahul Amin then provided a discussion of these two cases and important points when considering intermediate-risk patients for active surveillance. According to Dr. Mahul, the pathology report of the prostate needle biopsy is extremely critical for selecting the right patients for active surveillance and is even more critical in the management of patients with intermediate risk disease. There several considerations of pathological aspects for intermediate risk patients:
- Step 1: completeness of the pathology report and the specialization of the pathologist reading the report
- Step 2: the pathologist and urologist’s thorough understanding of the pathology report components that vital for appropriate patient selection
The current reporting guidelines for prostate cancer detected on needle biopsy include (i) histological type, (ii) Gleason score, (iii) Grade Group, (iv) percent grade 4 (for 3+4=7), and (v) percent grade 4/5 for Gleason Score >= 7. Additionally, it is important to note the number of positive cores, other atypical cores, and quantification of tumor in the involved cores. Finally, it is important to document (if identified) intraductal carcinoma and local invasion (peri-prostatic fat, seminal vesicle invasion, etc).
When discussing pattern 4 disease it is important to note that not all pattern 4 tumors are morphologically and biologically similar. Different morphologies include poorly formed glands, fused glands, cribriform glands, and glomeruloid glands: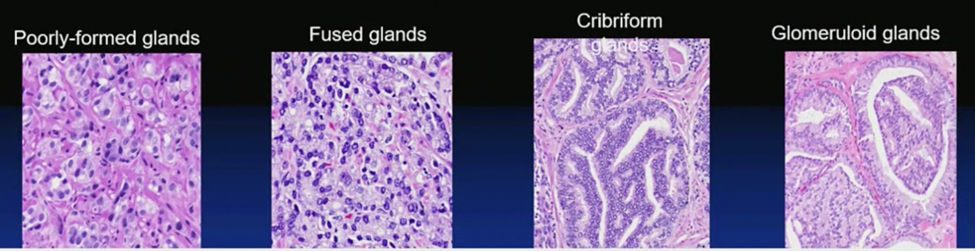
The cribriform pattern in prostate cancer is associated with worse outcomes than fused gland pattern Gleason pattern 4. It is also associated with higher rates of metastasis and death and has a different molecular profile with SPOP and FOXA1 mutations. Additionally, it has different methylation clusters, as well as PTEN and p27 loss with higher proliferation rates. Intraductal carcinoma of the prostate may be a late event in prostate cancer evolution, with the intraductal spread of aggressive prostate cancer and cancerization of pre-existing ducts and acini by high-grade prostate cancer. This entity is associated with high volume disease, frequent EPE and lymph node involvement, as well as higher rates of biochemical recurrence.
Presented by:
Nicola Fossati, MD, FEBU, Division of Oncology / Unit of Urology, IRCCS Ospedale San Raffaele - Ville Turro, Vita-Salute San Raffaele University, Milan, Italy;
Mahul B. Amin, MD, Chair of the Department of Pathology in the College of Medicine at the University of Tennessee Health Science Center (UTHSC). The UTHSC Gerwin Chair for cancer research. University of Tennessee Health Science Center, Memphis, Tennessee
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md at the 12th European Multidisciplinary Congress on Urological Cancers (EMUC) (#EMUC20 ), November 13th - 14th, 2020


