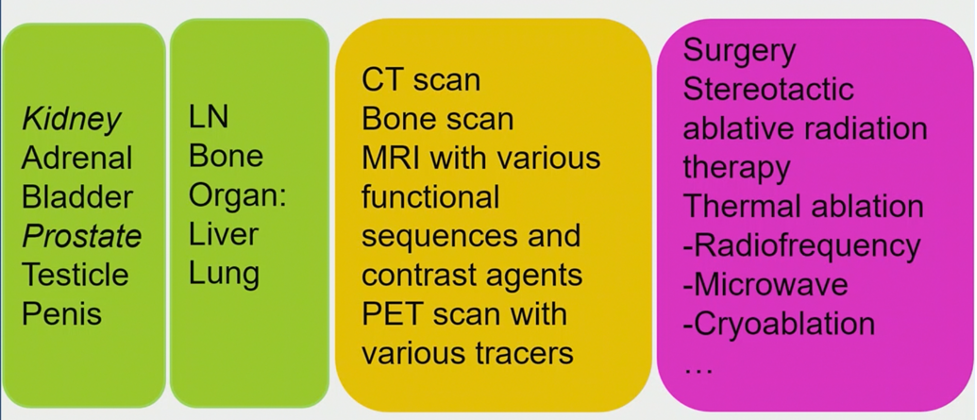
According to Dr. Thoeny, the problem of oligometastatic disease is delineating “true” oligometastatic disease (all metastases are reliably detected by imaging and treatment makes sense), and “false” oligometastatic disease (the real tumor burden is not detected by imaging and there is under or overdiagnosis). As such, reliable imaging needs to be combined with adequate targeted treatment. Dr. Thoeny states that for detecting liver and lung metastasis, MRI including DWI for the liver and CT scan for the lung should be used for assessment. For bone and lymph node detection, options include whole-body MRI and PET CT with various tracers. There are several prerequisites when considering imaging:
- Maximal sensitivity and specificity for disease detection
- Appropriate organ coverage
- Optimal timing and intensity of imaging follow-up
Dr. Thoeny notes that functional imaging precedes the detection of morphologically visible metastases. However, there are several challenges of functional imaging, including standardization, validation, expertise, training, quality control, availability, and reproducibility.
For detecting bone metastases in prostate cancer, PSMA PET is the most sensitive and specific method, with false-negative rates reported at ~5% secondary to absent or low expression of PSMA on prostate cancer cells. Of note, PSMA can be negative in advanced castration-resistant prostate cancer since metastases can lose PSMA expression. Dr. Thoeny notes that major drawbacks of PSMA PET imaging is the current high cost and limited availability. With regards to detecting lymph node metastases, PSMA PET CT is not as reliable compared to detecting bone metastases. Even though PSMA PET is superior to conventional imaging, pelvic lymph node dissection remains the gold standard.
Dr. Thoeny’s group previous prospectively assessed the diagnostic performance of diffusion-weighted (DW) magnetic resonance (MR) imaging in the detection of pelvic lymph node metastases in patients with prostate and/or bladder cancer staged as N0 with preoperative cross-sectional imaging.1 Among 4846 lymph nodes resected in 120 patients, 88 lymph node metastases were found in 33 of 120 patients (27.5%). The short-axis diameter of these metastases was less than or equal to 3 mm in 68, more than 3 mm to 5 mm in 13, more than 5 mm to 8 mm in five; and more than 8 mm in two. Thus, they concluded that DW MR imaging enables noninvasive detection of small lymph node metastases in normal-sized nodes in a substantial percentage of patients with prostate and bladder cancer diagnosed as N0 with conventional cross-sectional imaging techniques.
Dr. Thoeny states that for detecting lymph node metastases, functional imaging (DWI, USPIO-enhanced MRI, PET with various tracers) improves lymph node staging compared to morphological imaging only and guides the surgeon or radiation oncologist with respect to treatment. However, in her opinion, the optimal imaging method to detect micrometastases does not exist as of yet and thus extended pelvic lymph node dissection remains standard of care.
Dr. Thoeny summarized her presentation with the following take-home messages:
- Correct selection of the patient for the adequate imaging method depends on the histological type and grade of the tumor
- The adequate imaging method is the prerequisite for the detection of the true extent of oligometastatic disease allowing personalized treatment
- Bone metastases: for prostate cancer PSMA PET is the best modality
- Lymph node metastases: there is no ideal imaging technique to detect micrometastases, however, there are promising results with DWI, USPIO-enhanced MRI (+DWI), and PSMA-PET
Presented by: Harriet Thoeny, MD, Ph.D., Full professor of radiology, University of Fribourg, Fribourg, Switzerland
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Twitter: @zklaassen_md at the 12th European Multidisciplinary Congress on Urological Cancers (EMUC) (#EMUC20 ), November 13th - 14th, 2020
References:
1. Thoeny HC, Froehlich JM, Triantafyllou M, et al. Metastases in normal-sized pelvic lymph nodes: detection with diffusion-weighted MR imaging. Radiology. 2014 Oct;273(1):125-135.


