To assess this, the authors utilized data from Medicare (MC) and Veterans Health Administration (VA) cohorts. They captured patient characteristics, treatment patterns, and OS in men with mCSPC treated with androgen deprivation therapy (ADT) ± first generation non-steroidal antiandrogens (NSAA), DOC, or NHT from 2010 to 2018 (MC) / 2019 (VA).
They used Kaplan-Meier and Cox models adjusting for baseline characteristics to estimate overall survival in 3 cohorts: those treated before (2010–2011) and after (2012–2014) guideline recommendations for NHT use in metastatic castration-resistant prostate cancer (mCRPC) and after recommendations for DOC or NHT in mCSPC (2015–2018/2019).
They identified 33,641 men with mCSPC in the Medicare cohort and 5,651 men in the VA cohort who had a mean age of 76.6 and 73.0, respectively. While patient characteristics were generally similar over time, there was increasing prevalence of nodal metastases.
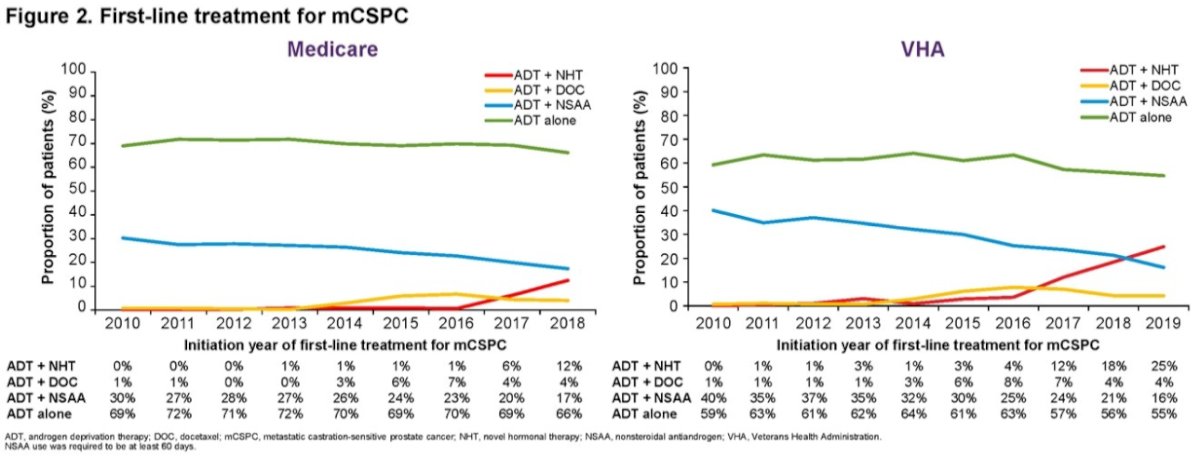
Over time, the use of ADT alone and ADT + NSAA declined, and the use of ADT + DOC and ADT + NHT increased, though they remained low. Even as of 2018/2019, less than one-third of patients with mCSPC received first-line ADT + DOC or ADT + NHT.
While there were changes in treatment approaches between 2010 and 2014, the authors did not find any changes in overall survival in 2012–2014 compared with 2010–2011, though there was improvement in overall survival by 12% and 15% in MC and the VA, respectively, in 2015–2018/2019 vs 2010–2011, after adjusting for baseline characteristics.
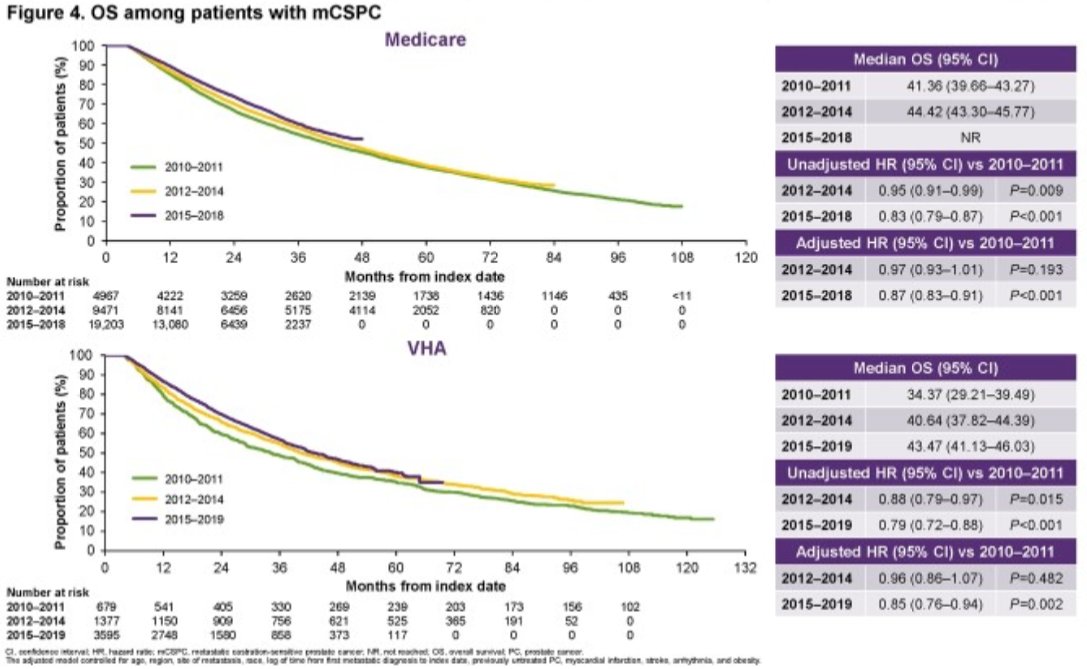
The authors noted that improvements in overall survival in men treated for mCSPC between 2015 and 2018/19 coincided with the use of treatment intensification in this disease space. However, ongoing underutilization suggests that additional, population-level, survival benefits may be realized.
Presented by: Daniel George, MD, Duke Cancer Institute, Durham, NC
Written by: Christopher J.D. Wallis, University of Toronto Twitter: @WallisCJD during the 2022 European Society of Medical Oncology (ESMO) Annual Hybrid Meeting, Paris, FR, Fri, Sept 9 – Tues, Sept 13, 2022.


