She began with a short introduction on prostate-specific membrane antigen (PSMA), building on the presentation from Dr. Bander. She began by noting that PSMA is a type II transmembrane protein that is a promising and specific target for prostate cancer imaging. This is because it is between 100 and 1000 times over-expressed on prostate cancer cells. This makes it an excellent target for both diagnosis and therapy. Additionally, as expression correlates with unfavorable prognostic factors, quantitative assessment may provide prognostic information. However, it bears nothing that approximately 10% of all primary prostate cancers will be PSMA-PET negative.
Beginning in 2017, work from Dr. Eiber and colleagues demonstrated the breadth of radiotracers that were already available at that time including those that are 68Ga-labelled and those that are 18F-labelled. Examples of each of these have gained relatively widespread uptake.
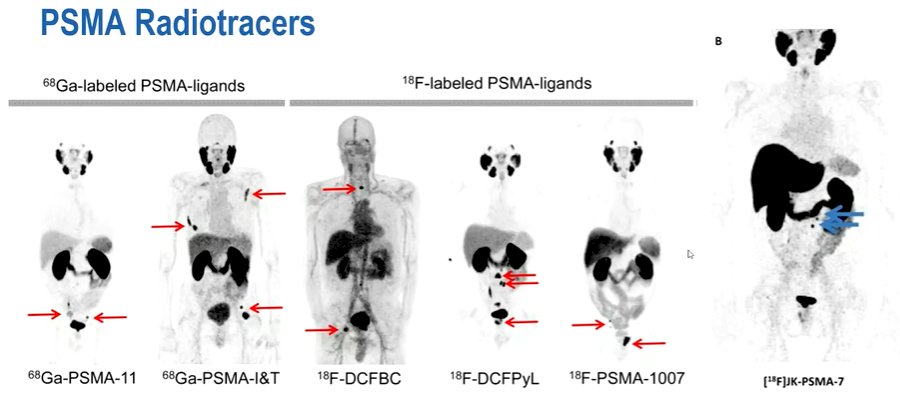
She noted that the biodistribution is generally comparable between these with physiologic uptake in the lacrimal and salivary glands, as well as renal uptake with genitourinary excretion (apart from 18F-PSMA-1007). Uptake in the liver and spleen is somewhat variable between the tracers.
She noted at least three important differences between the 68Ga- and 18F-labelled tracers. First, 18F-labelled radiotracers have a substantially longer half-life. Second, she noted that the 68Ga-labelled tracers are generator products, requiring production on site. In contrast, 18F-labelled radiotracers are cyclotron products that may be produced on a larger scale for distribution. Third, she noted that 18F-labelled radiotracers may have a better tumor:background ratio, potentially allowing for better image resolution.
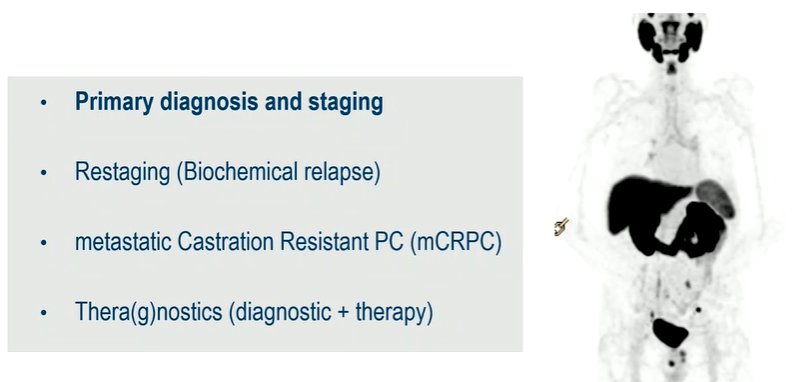
She next noted that PSMA-PET imaging may be used for a variety of indications in the care of patients with prostate cancer including primary diagnosis and staging, restaging at the time of biochemical relapse, the evaluation of patients with metastatic castration-resistant disease, and in a theranostic setting.
She focused next on its role in primary diagnosis and staging. In this context, she noted that fewer than 10% of patients newly diagnosed with prostate cancer will have metastatic disease. However, imaging is essential to exclude distant metastases before embarking on local therapy in patients with intermediate and high-risk disease. Further, in patients found to have oligometastatic disease, there is a potential benefit to combining primary prostate-directed treatment with loco-regional metastasis-directed therapy.
She noted that, when used in this setting, PSMA-PET will often only show activity within the prostate cancer. She suggested that nuclear medicine physicians may provide some information regarding the risk of extracapsular spread or invasion of the seminal vesicles. However, many patients will have evidence of variable PSMA activity, indicative of nodal or bony metastatic spread.
She noted the first dilemma that may arise in these patients: the “bone scan dilemma” in whom there is no evidence of metastatic disease on conventional imaging (eg. bone scan) but who have evidence of metastatic disease on PSMA-PET imaging. She raised the question of how we may reconcile these results. A similar issue arises in terms of CT imaging with respect to both lymphadenopathy and bony lesions. There may be PSMA-avid lesions seen on PSMA-PET where CT imaging shows only very small lesions (3-4cm). Further, PSMA-PET may identify bony lesions in which a CT correlate is more consistent with tiny sclerotic lesions or indeed no lesion at all.
To address these comparative issues, she noted results of the proPSMA trial that were published by Dr. Hofman and colleagues comparing conventional imaging with PSMA-PET-based staging prior to treatment of presumed high-risk localized prostate cancer. This prospective, randomized trial provided evidence that PSMA-PET imaging had superior activity, greater treatment impact, fewer uncertain results, as well as less exposure to radiation.
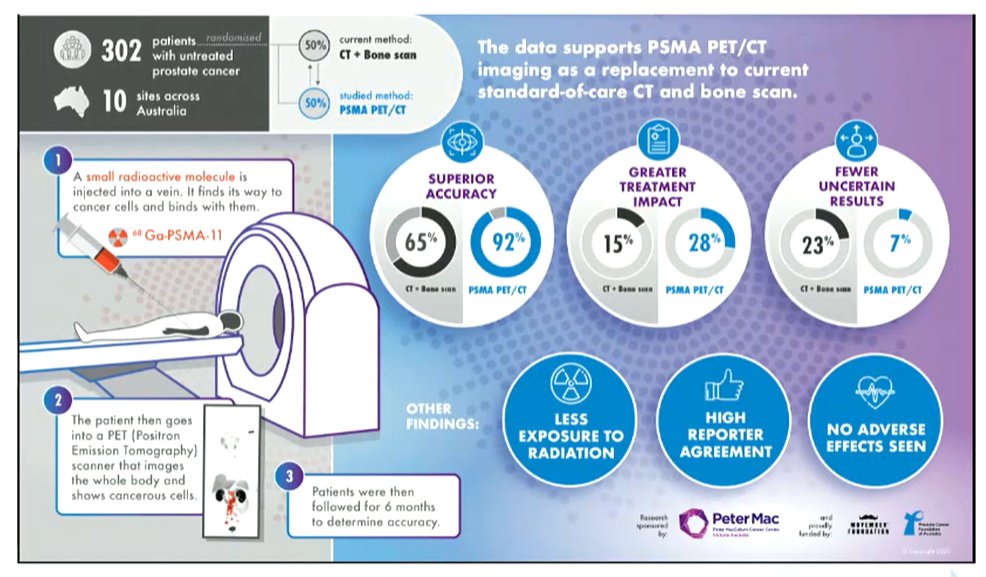
On this basis, as of 2021, the EAU guidelines state that PSMA-PET/CT is more accurate for staging than conventional imaging in high-risk disease while acknowledging that there is no subsequent outcome data regarding management. Notably, when using PSMA-PET, the guideline body provided a strong rating that we must be aware of the lack of outcome data to inform subsequent treatment changes.

Thus, she emphasized that it is unclear whether “seeing more” and “doing more” and treating more sites of disease, whether there is an outcome benefit for patients.
Thus, she concluded that Pandora’s box is now open: we cannot ignore modern imaging approaches. However, it is somewhat unclear on how we should act on their results and we need to provide evidence of improvements in clinically meaningful outcomes for our patients.
Presented by: Daniela Oprea-Lager, Cancer Center Amsterdam, Amsterdam, NetherlandsWritten by: Christopher J.D. Wallis, University of Toronto Twitter: @WallisCJD during the 2022 European Society for Medical Oncology (ESMO) Annual Congress, 9-13 September 2022.


