(UroToday.com) On Monday, September 12, 2022, in Presidential Symposium III at the European Society for Medical Oncology (ESMO) Annual Congress, Dr. Parker presented results of the RADICALS-HD trial examining the effect of differing durations of androgen deprivation therapy (ADT) among men receiving post-operative radiotherapy following radical prostatectomy for prostate cancer. This is a key question as, though there is substantial high-quality evidence regarding the role and durations of ADT for men receiving primary radiotherapy for the treatment of prostate cancer, there is considerable uncertainty regarding its role and duration for men who are receiving post-prostatectomy radiotherapy.
To address this, the authors designed the RADICALS-HD trial, a randomized comparison assessing questions regarding the use and duration of ADT with postoperative radiotherapy, within the RADICALS protocol which also addressed questions relating to the timing of radiotherapy (adjuvant versus early salvage) (ISRCTN40814031). The investigators enrolled men with an indication for post-operative radiotherapy who had not received previous post-operative ADT. Notably, those with prior pelvic RT, prior hormonal therapy, metastatic disease, or a PSA over 5 ng/mL were excluded.
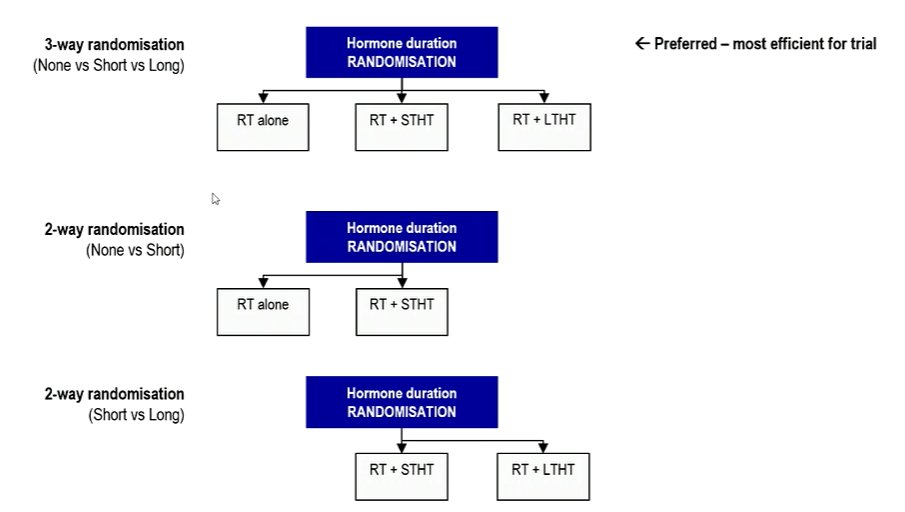
Following radical prostatectomy but prior to the initiation of their radiotherapy, patients were randomised to either no ADT (“None”), 6mo ADT (“Short”), or 24mo ADT (“Long”). While, 3-way randomisation was encouraged (to all of the treatment options), 2-way randomisation between both None-vs-Short or Short-vs-Long also allowed.
The trial was powered for the two pairwise comparisons. The primary outcome measure was metastasis-free survival (MFS) with secondary outcomes including time to salvage ADT and overall survival (OS).

Toxicity assessments focused on RT with RTOG scale. All confidence intervals (CI) are 95%.
Between 2007 and 2015, 2839 patients were enrolled in RADICALS-HD from UK, Canada & Denmark. The median age of included men was 66 years and, in terms of cancer characteristics, 23% had pT3b/T4 disease stage, 20% had Gleason 8-10 histology, and the median pre-RT PSA was 0.22ng/ml (consistent with an early salvage treatment intent).
Of the 2389 patients in RADICALS-HD, 492 participated in the 3-way randomisation. Including both 2-way and 3-way randomization, 1480 patients contributed to the None-vs-Short comparison and 1523 patients contributed to the Short-vs-Long comparisons.
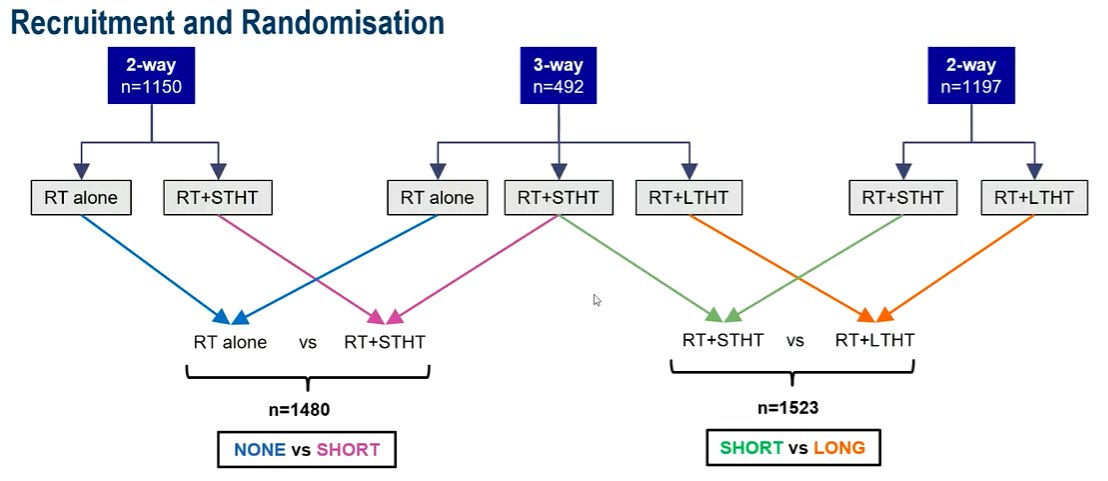
Arms were balanced within each comparison; risk factors were more favourable in None-vs-Short than Short-vs-Long, in keeping with self selection for a two-way randomization.
Over a median follow-up of 9 years, in None-vs-Short comparison, based on 268 MFS events, 6 months of ADT did not improve MFS compared to no ADT (HR 0.89; CI: 0.69-1.14; 79% vs 80% event-free at 10 years).
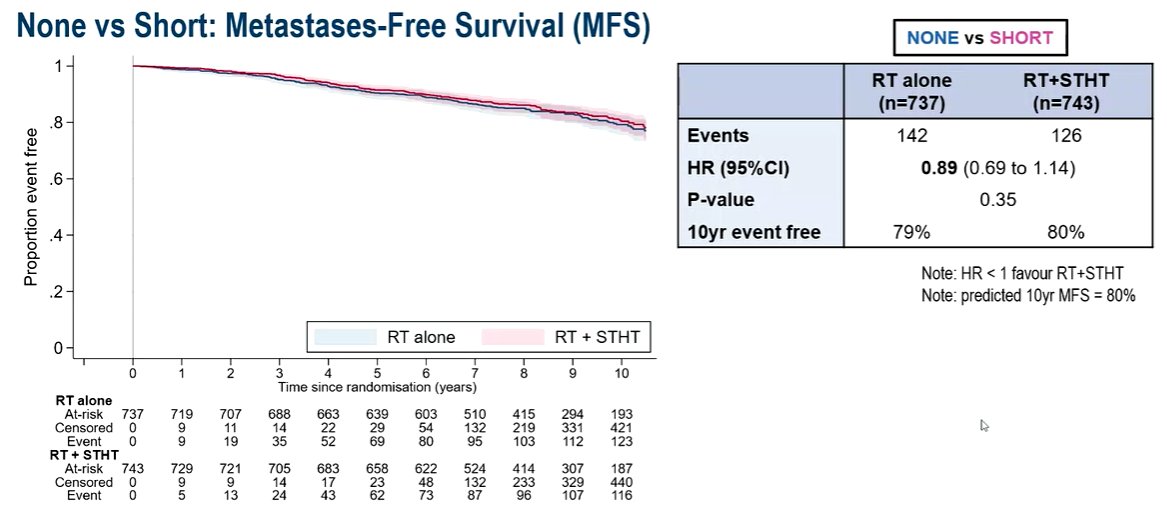
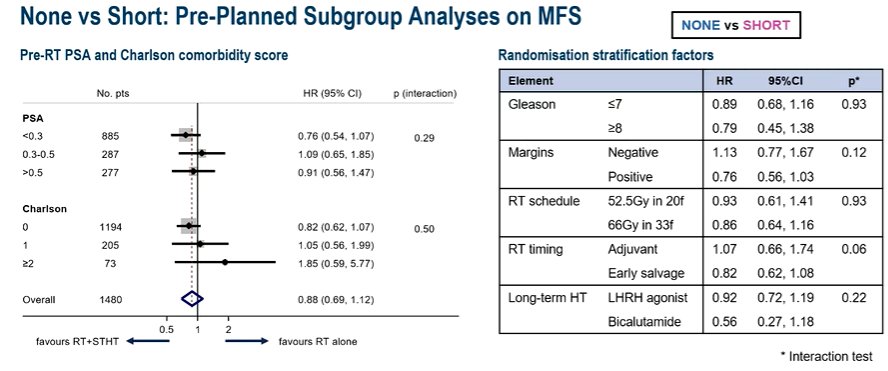
Similarly, OS was not improved (HR 0.88; CI: 0.65-1.19) nor was freedom-from-distant-metastasis (HR 0.82; CI: 0.58-1.15. However, the time to salvage ADT was delayed (HR 0.54; CI: 0.42-0.70). Pre-planned subgroup analyses failed to demonstrate any significant effect modification according to pre-RT PSA, comorbidity, or randomization stratification factors.
In the comparison of Short-vs-Long duration of ADT, based on 313 MFS events, 24 months of ADT improved MFS (HR 0.77; CI: 0.61-0.97; 72% vs 78% at 10yrs), freedom-from-distant-metastases (HR 0.63; CI:0.47-0.85), and delayed the time to salvage ADT (HR 0.73; CI: 0.59-0.91).
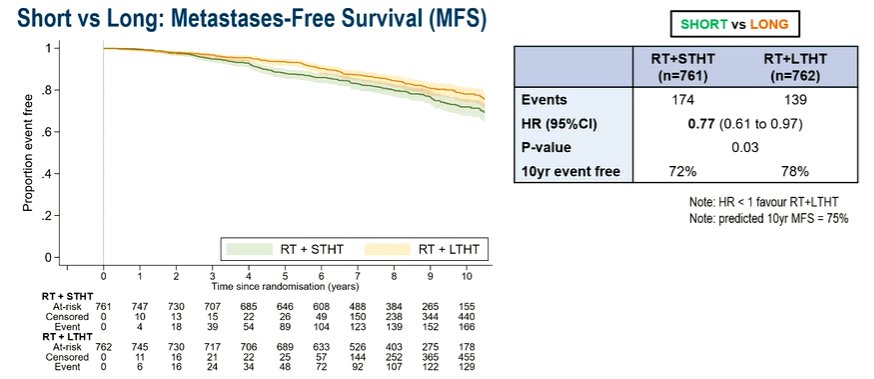
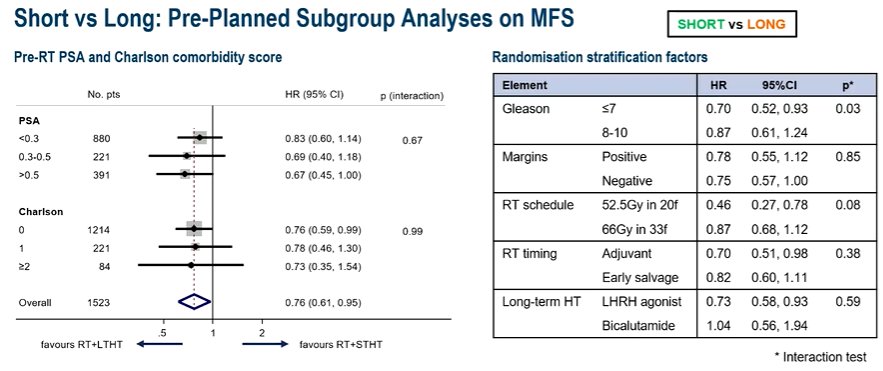
However, OS was not improved (HR 0.88; CI: 0.66-1.17). In pre-planned subgroup analyses, there was some heterogeneity of effect with a statistically significantly greater benefit seen in patients with Gleason score of 7 or less.
While the results may seem intuitive, Dr. Parker then presented results of the none versus long comparison. Interestingly, there was no difference in metastasis-free survival seen (HR 0.94; CI:0.53-1.68).
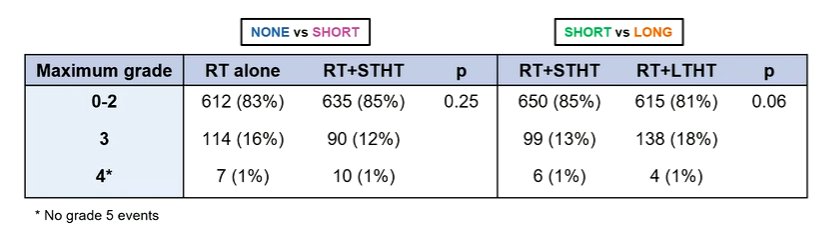
He further noted that, across both comparisons, there was no statistically significant increase in toxicity as measured using RTOG grades.
Considering the applicability of these data, Dr. Parker noted that this is a large, international RCT, with more than 9 years of follow-up. However, overall survival data remain immature and practice patterns have shifted such that early salvage therapy is now preferred over adjuvant and pelvic nodal radiation is being increasingly used in this setting.
Thus, Dr. Parker concluded that, among patients undergoing radiotherapy following radical prostatectomy, the use of 24 months of ADT improved both metastasis-free survival and the time to salvage ADT. However, 6 months of ADT (compared to none) provided only a benefit in the time to salvage ADT, without improvements in metastasis-free survival.
Presented by: Chris C. Parker, MD, FRCR, MRCP, National Cancer Research Institute Prostate Clinical Studies Group, Sutton, UKWritten by: Christopher J.D. Wallis, University of Toronto Twitter: @WallisCJD during the 2022 European Society for Medical Oncology (ESMO) Annual Congress, 9-13 September 2022.


