Summarizing these data, he noted that they, together, represent the challenges and opportunities present in the treatment of rare genitourinary cancers.
He began by noting that the updated version of the international germ cell cancer collaborative group (IGCCCG) Update demonstrates the value of collective international collaborative efforts. As of the 2021 publication, this work has validated the original classification and added additional nuance to the model with the inclusion of age and lung metastasis as prognostic features in non-seminoma. In the data presented at this year’s ESMO, the authors used this data set to address the prognosis of patients with relapse versus de novo metastatic germ cell tumors.
This is important as, in other GU cancers, patients with synchronous metastatic disease are known to do substantially worse than those with relapsed disease – including for example both metastatic castration sensitive prostate cancer and metastatic renal cell carcinoma. However, in germ cell tumors, we lack this data. However, a surveillance has been widely adopted in patients with clinical stage I testis cancer. To this end, he highlighted the ESMO-EUROCAN clinical practice guidelines which emphasize the appropriateness of active surveillance for those with low-risk, stage I non-seminoma. While treatment can be offered, in these patients, relapse rates are relatively low (10-12%) and thus there is a meaningful risk of overtreatment. In patients with high-risk disease, relapse rates are 40 to 50% and thus a single cycle of BEP is often advised. Notably, he emphasized that the classical teaching has been that 95% of patients would have good prognosis at the time of relapse.
In the context of stage I seminoma, he noted that survival is high regardless of approach, thus surveillance is more widely recommended. However, carboplatin may be considered adjuvantly in higher-risk patients including those with larger tumors (>4cm) and those with rete testes invasion.
Back to the data presented at this year’s ESMO, he noted that the distribution of risk on the relapsed CSI non-seminoma patients should 82% with good risk disease and the remainder with intermediate or poor-risk disease, suggesting a somewhat more aggressive distribution that has previously been noted.
When adjusting for IGCCCG risk, he noted that “reassuringly” outcomes are similar for patients with metastatic disease following relapse as for those with de novo metastatic disease. A similar story was observed for seminoma, with evidence of difference in risk groups.
As a take away from this study, he noted that active surveillance is widely recommended those guidelines are not identical. While the distribution of patients at relapse following initial surveillance for CSI disease was more aggressive than classical assumptions, he emphasized that this should not be used to advocate for more adjuvant therapy. Instead, effective treatment at relapse is critical to optimize outcomes. However, these data do not fully examine outcomes for patients following adjuvant therapy.
(UroToday.com) Moving to data presented by Dr. Jansson, he noted the strengths of the data from Sweden with largely government-funded care. However, at the time of study accrual, 8 to 9% of cases had a psychiatric diagnosis coded. He suggested that, in the interim, rates of diagnoses of neurodevelopmental disorders have likely risen, potentially as a result of better recognition.
Importantly, Dr. Jansson and colleagues found an association between a history of neurodevelopmental disorders and seminoma, as well as evidence of a younger age at diagnosis and more advanced stage of disease at diagnosis. Dr. Lalani suggested, however, that these differences in age may not have clinical implications to care.
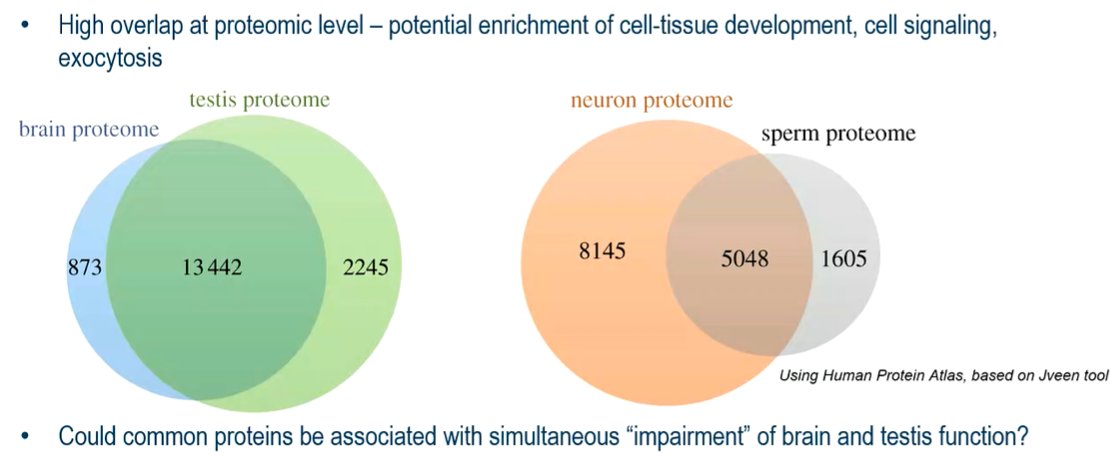
The authors also found higher rates of all-cause and cause-specific mortality (for both seminoma and non-seminoma) among those men with a history of psychiatric diagnosis. This highlights these patients as an at-risk subgroup. He suggested that the brain and testes may both have biological overlap. When explored at a proteomic level, there is potentially high overlap in terms of cell-tissue development, cell signaling, and exocytosis.
He highlighted numerous other potential explanations including unmeasured factors, social and access to care issues (including both prior to diagnosis and following diagnosis), as well as how to biologically reconcile the disparate findings in terms of seminoma and non-seminoma. Broadly speaking, he noted that individuals with mental health illnesses often have shorter life-expectancy and have increased mortality following cancer diagnosis. This may act through numerous pathways including neurohormonal factors, functional/emotional impairments, and implications for other care determinants.
Finally, he moved to discussing results from Dr. Chahoud regarding the role of neoadjuvant chemotherapy in penile squamous cell carcinoma. Dr. Lalani noted that penile cancer is an orphaned disease, owing to its rarity. This creates issues in terms of limited available data to guide care, risk of patient selection bias, and referral bias. He emphasized the variation in rates of diagnosis of penile cancer globally on the basis of geography. While the association between HPV and penile cancer is well known, precise tumorigenesis remains to be elucidated. The lack of understanding of the biology has limited targeting of therapies.
He noted that the most recent EAU guidelines have recommended neoadjuvant chemotherapy in patients with T4 and cN3 disease. The rationale for neoadjuvant chemotherapy is premised on the early treatment of systemic disease with down-sizing of lymph node metastases. On the basis of phase II data, TIP (paclitaxel, ifosfamide, and cisplatin) has been fairly widely adopted as systemic therapy in this setting.
To address many of these issues, the authors performed a large, multi-institutional cohort study. Dr. Lalani emphasized that there is important representation of patients from South America as well as a large sample size. He noted that more than 1 in 10 patients had a complete response. He noted these as “impressive” data.
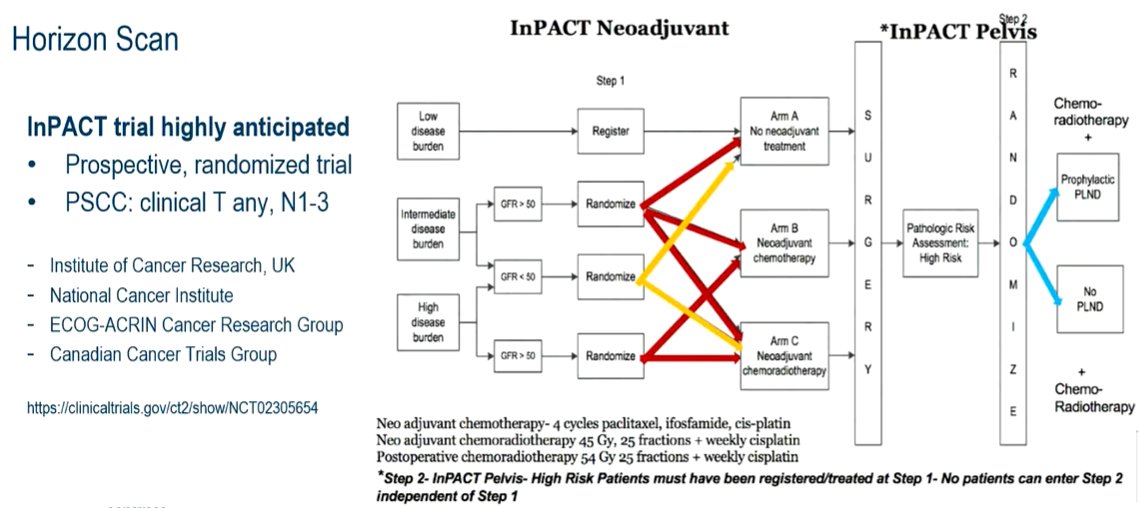
As take-aways, he emphasized that penile cancer care often requires multi-disciplinary input given its rarity and complexity and thus is best managed as high-volume centers. Neoadjuvant TIP is the standard of care though future correlative work is important to better understand the disease biology and target treatment approaches. He highlighted the ongoing InPACT trial which will hopefully add substantially to the body of knowledge in the care of these patients.
Presented by: Aly-Khan Lalani, MD, Assistant Professor at McMaster University, Ontario, CA


