(UroToday.com) The 2023 ESMO annual meeting included a session on prostate cancer, featuring a presentation by Dr. Noel Clarke discussing the final results of the RADICALS RT randomized clinical trial. The optimal timing of radiotherapy after radical prostatectomy for prostate cancer is uncertain, thus the RADICALS-RT trial compared the efficacy and safety of adjuvant radiotherapy versus an observation policy with salvage radiotherapy for early PSA failure.1
Dr. Clarke and colleagues previously reported the early outcome measure of biochemical PFS, concluding that there was no evidence of a difference in outcomes with post-radical prostatectomy adjuvant and salvage radiotherapy. Furthermore, a high proportion of men did not require treatment post-radical prostatectomy, and adverse effects from adjuvant radiotherapy were greater than for salvage radiotherapy. Now, there are enough events to report on the primary outcome of freedom from distant metastases.
Patients with post-op PSA ≤ 0.2ng/ml and ≥ 1 risk factor (pT3/4, Gleason 7-10, positive margins, or pre-op PSA ≥ 10ng/ml) were randomized ≤ 22 weeks after radical prostatectomy to adjuvant radiotherapy or observation + salvage radiotherapy for PSA failure: PSA ≥ 0.1ng/ml or three consecutive rises. The trial design for RADICALS-RT is as follows:

Stratification factors were Gleason score, margin status, planned radiotherapy volume (prostate bed only, prostate bed + pelvis), radiotherapy schedule (52.5 Gy/20f, 66 Gy/33f), and center. The primary outcome was freedom from distant metastases with >1,200 patients needed for 80% power to detect an improvement from 90% to 95% at 10 years with adjuvant radiotherapy. Secondary outcomes include overall survival, safety, and patient reported outcomes (1, 5, and 10 years). Biochemical progression free survival was defined as the first of:
- PSA >= 0.4 ng/mL following radiotherapy
- PSA > 2.0 ng/mL at any time
- Clinical progression
- Initiation of non-protocol hormone therapy
- Death from prostate cancer
There were 1,396 patients randomized (697 to adjuvant radiotherapy, and 699 to observation + salvage radiotherapy) from October 2007 to December 2016 (82% in the UK, 13% in Denmark, 4% in Canada, and 1% in Ireland). The accrual by year is as follows: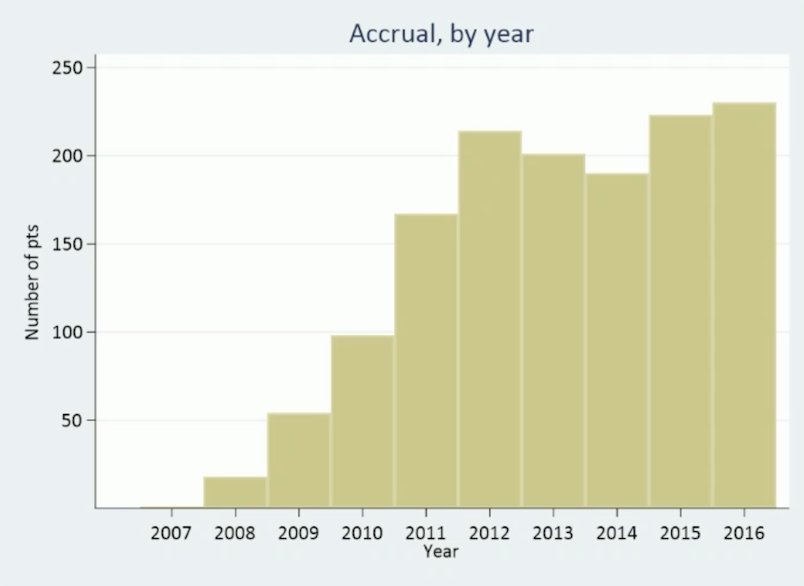
The median age was 65 years and 37% (517/1,396) had a CAPRA-S score of 6+. Data were frozen in May 2022 and median follow-up was 8 years. Overall, 93% (650/697) underwent adjuvant radiotherapy and started radiotherapy within 5 months and 39% (270/699) underwent observation + salvage radiotherapy and started radiotherapy:
The median PSA at time of salvage radiotherapy was 0.2 ng/ml, and 24% (156/650) of men undergoing adjuvant radiotherapy and 27% (72/270) undergoing observation + salvage radiotherapy reported hormone therapy with their radiotherapy. With 80 events, freedom from distant metastases at 10 years was 92.7% for adjuvant radiotherapy versus 89.6% for observation + salvage radiotherapy (HR 0.68, 95% CI 0.43 to 1.07):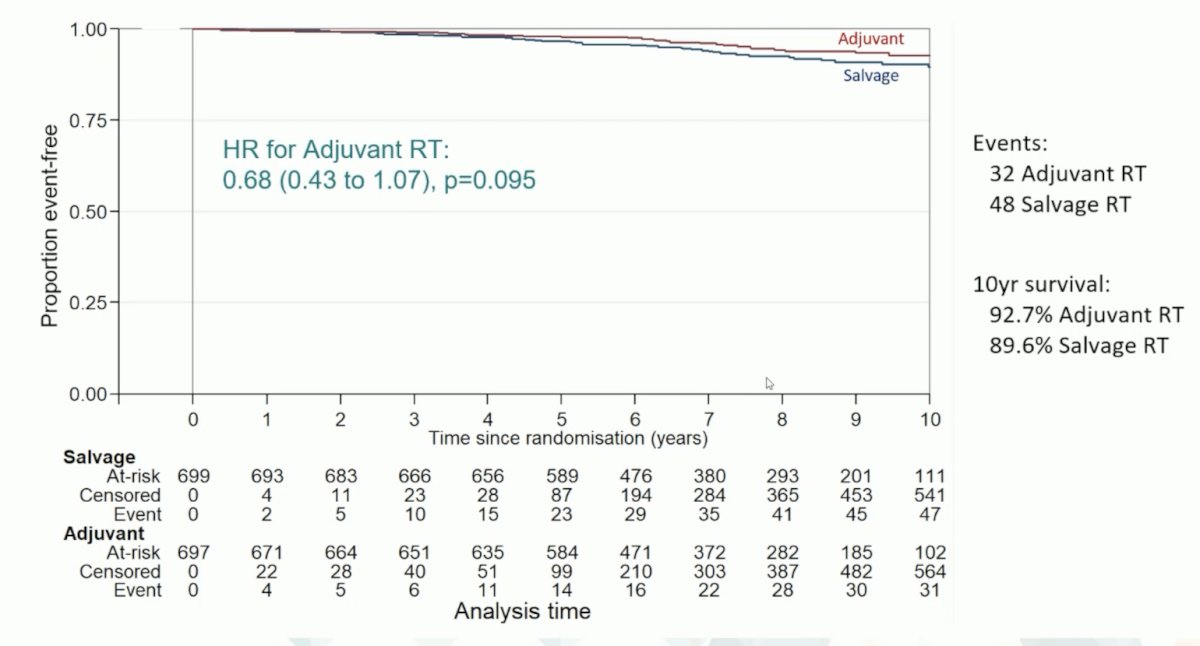
Overall survival at 10-years was 87.6% vs 87.4% (HR 0.98, 95% CI 0.67 to 1.44):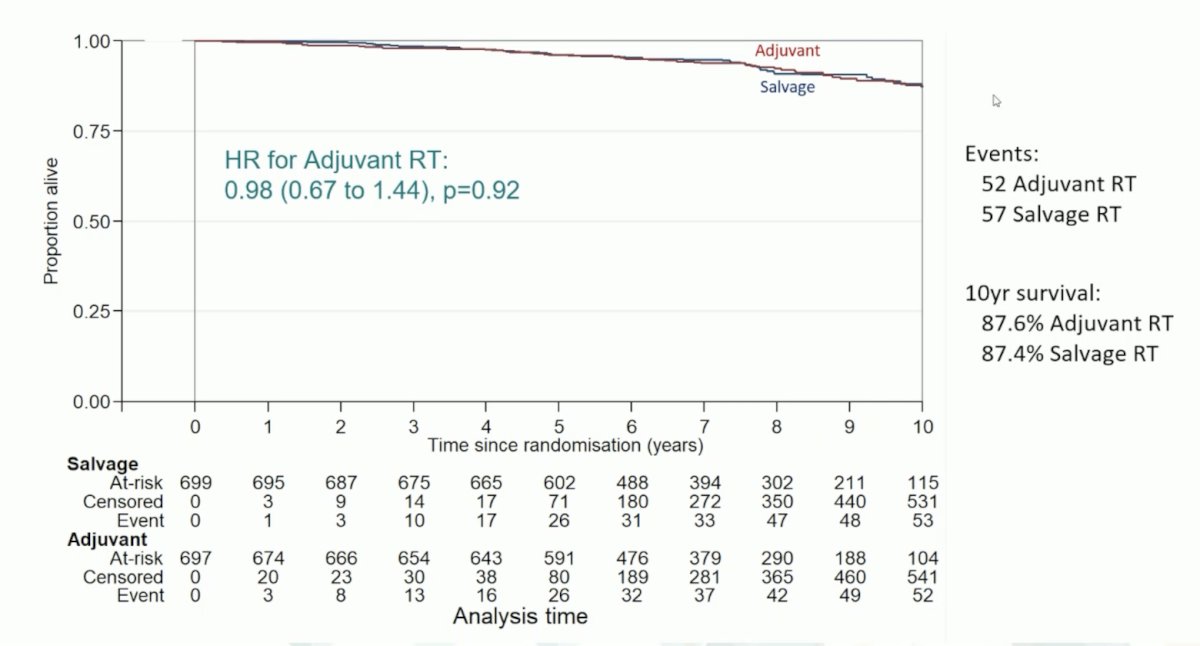
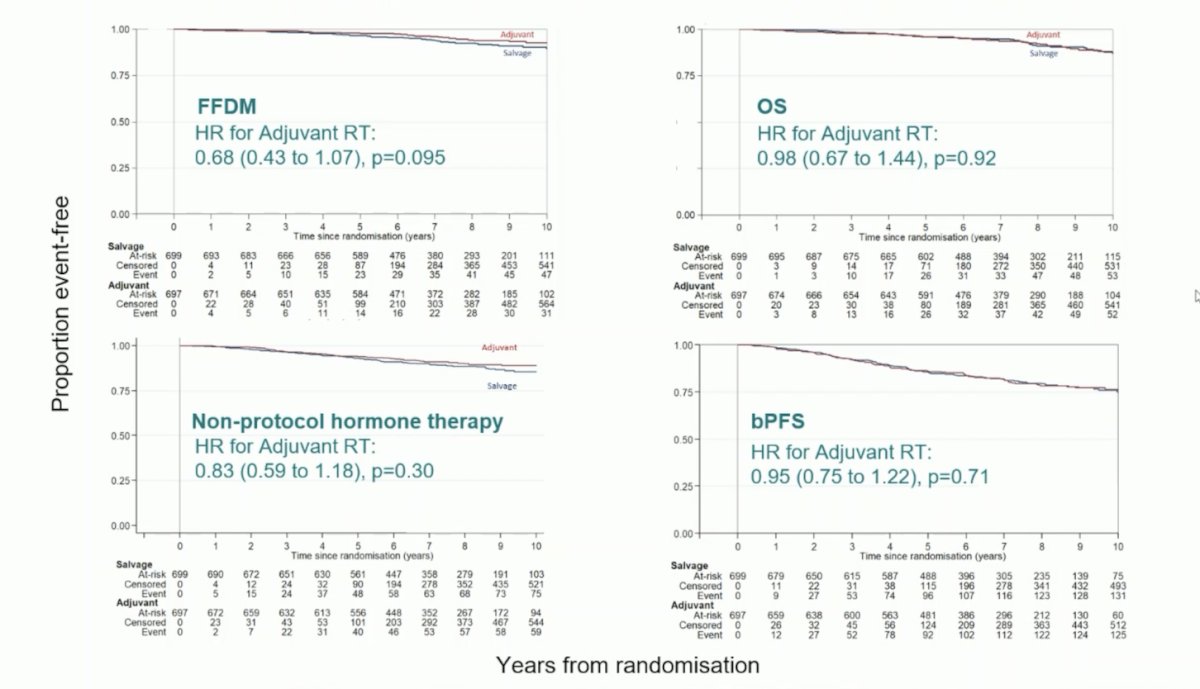
Following are the results from freedom from distant metastasis, overall survival, non-protocol hormone therapy, and biochemical progression free survival:
Both urinary and gastrointestinal toxicity, based on the RTOG scale, were worse with adjuvant as compared to salvage radiotherapy: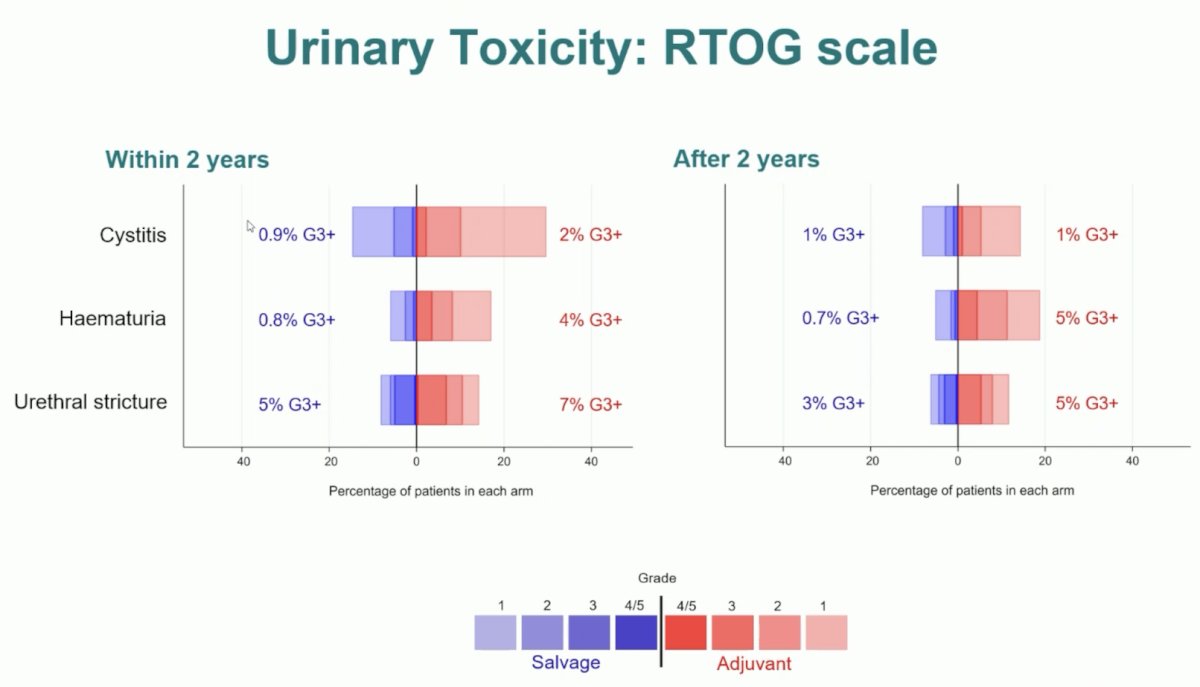
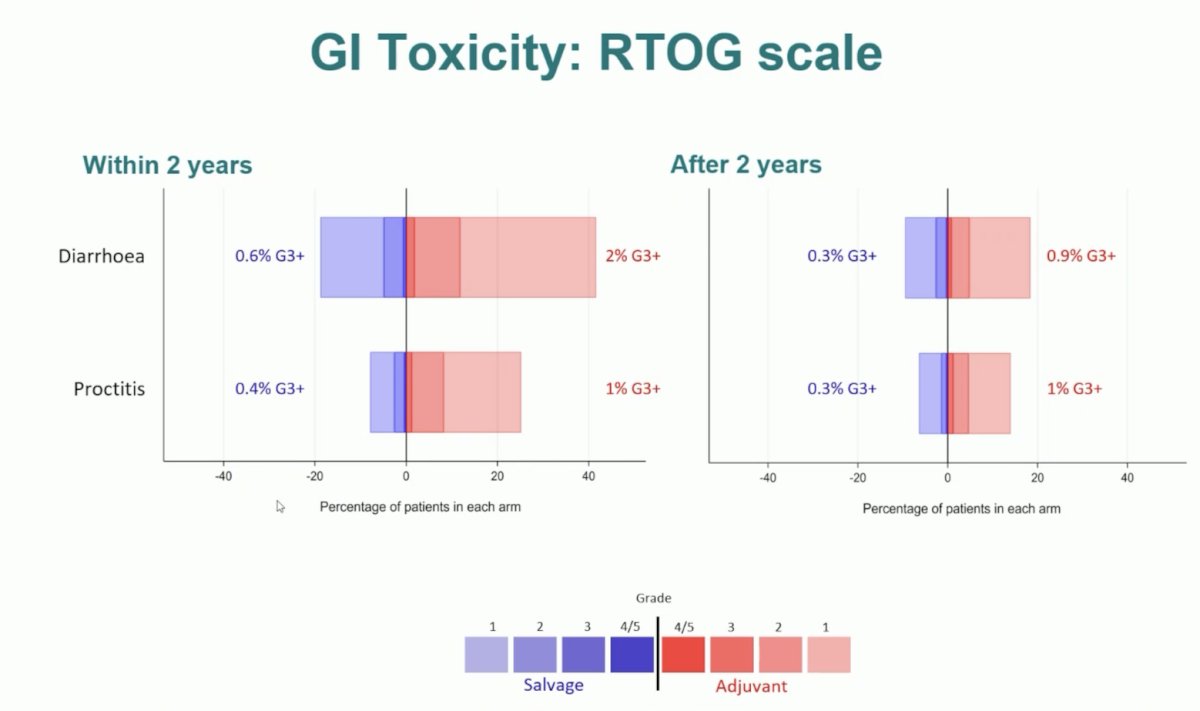
Self-reported urinary incontinence and fecal incontinence were worse at 1 year for adjuvant radiotherapy (p<0.001).
Dr. Clarke concluded his presentation discussing the final results of the RADICALS RT randomized clinical trial with the following take-home points:
- Long-term biochemical PFS and time to further hormone therapy were similar for the adjuvant and early salvage radiotherapy groups
- Early salvage radiotherapy is as effective as adjuvant radiotherapy regarding long term freedom from distant metastasis and overall survival
- Adjuvant radiotherapy had higher long-term urinary and bowel morbidity
- A larger proportion of men randomized to early salvage radiotherapy did not need radiotherapy in the long term
- RADICALS results support the use of early salvage radiotherapy for PSA failure after radical prostatectomy rather than early adjuvant intervention
Presented by: Noel Clarke, MBBS, FRCS, ChM, Manchester, United Kingdom
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2023 European Society of Medical Oncology (ESMO) Annual Meeting, Madrid, Spain, Fri, Oct 20 – Tues, Oct 24, 2023.
References:

