(UroToday.com)The 2023 ESMO annual meeting included a session on management of (very) high-risk localized prostate cancer, featuring a presentation by Dr. Alberto Bossi discussing dose intensification and field expansion of External Beam Radiation Therapy (EBRT). Dr. Bossi started by noting that high risk patients are the ideal candidates for selective intra-prostatic dose intensification:

Dr. Bossi then discussed the FLAME trial, which evaluated the role of additional focal boost to the MRI-visible lesion. In this randomized phase III trial, 571 patients with intermediate and high-risk prostate cancer received standard treatment at 77 Gy (2.2 Gy/fraction) to the entire prostate, with patients in the experimental arm receiving an additional simultaneous integrated focal boost up to 96 Gy (2.7 Gy/fraction) to the intraprostatic lesion visible on MRI. Organ at risk constraints were prioritized over the focal boost dose. The primary outcome was 5-year biochemical disease-free survival. After a median follow-up of 72 months, biochemical disease-free survival was superior in the experimental arm (HR: 0.45, 95% CI: 0.28 – 0.71, p<0.001), with 5-year rates of 92% and 85%, respectively.
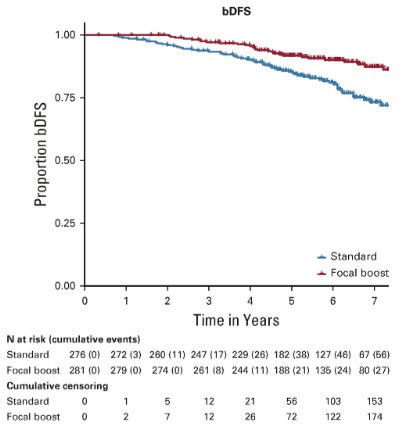
No difference was noted in the secondary, underpowered endpoints of prostate cancer-specific and overall survival. There were no significant differences in the cumulative incidence rates of grade 2+ late genitourinary (23% versus 28%) or gastrointestinal (12% versus 13%) toxicity between the standard and focal boost arms, respectively. Similarly, no difference in health-related quality of life was noted.
In 2018, Kishan and colleagues compared radical prostatectomy, external beam radiotherapy, or external beam radiotherapy with brachytherapy boost and disease progression and mortality in patients with Gleason score 9-10 disease.2 Among 1,809 men across 12 tertiary centers, 639 underwent radical prostatectomy, 734 EBRT, and 436 EBRT + brachytherapy boost. The median follow-up was 4.2, 5.1, and 6.3 years, respectively. By 10 years, 91 radical prostatectomy, 186 EBRT, and 90 EBRT + brachytherapy boost patients had died. Adjusted 5-year prostate cancer-specific mortality rates were radical prostatectomy 12% (95% CI, 8%-17%), EBRT 13% (95% CI, 8%-19%), and EBRT + brachytherapy boost 3% (95% CI, 1%-5%). EBRT + brachytherapy boost was associated with significantly lower prostate cancer-specific mortality than either radical prostatectomy or EBRT (cause-specific HRs of 0.38 (95% CI 0.21-0.68) and 0.41 (95% CI, 0.24-0.71)).
Results of the POP-RT trial were published in 2021 and highlighted by Dr. Bossi.3 This phase III trial randomized 224 prostate cancer patients with clinically node negative disease and an estimated nodal risk ≥ 20% to either prostate-only radiation therapy (68 Gy in 25 fractions) or whole pelvic radiotherapy (68 Gy in 25 fractions to the prostate plus 50 Gy to the pelvic nodes, including common iliac). All patients received image-guided, intensity-modulated radiotherapy and a minimum of two years of ADT. The primary end point was 5-year biochemical failure-free survival. Over a median follow-up of 68 months, the 5-year biochemical failure-free survival was superior in the whole pelvis arm (95% versus 81.2%; HR: 0.23; p < 0.001) as were 5-year disease-free (89.5% versus 77.2%; HR: 0.40, p = 0.002) and distant metastasis-free survivals (95.9% versus 89.2%; HR: 0.35, p = 0.01):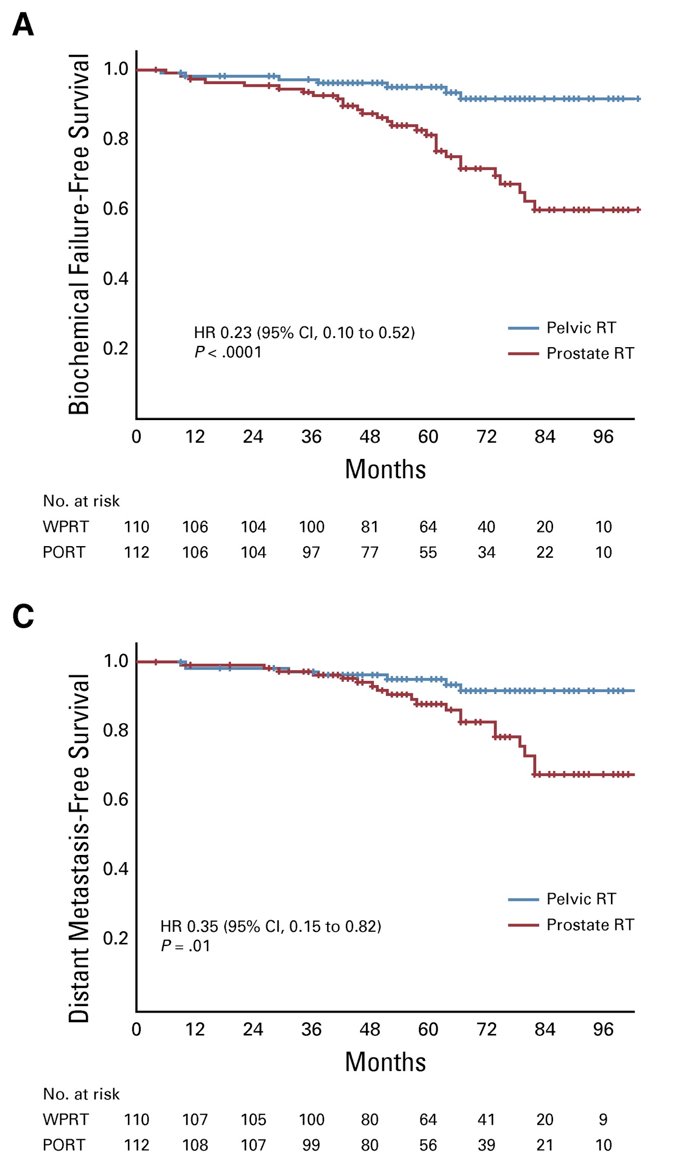
Additionally, patterns of recurrence in the POP-RT trial were as follows, highlighting that whole pelvic radiotherapy essentially eliminated the likelihood of nodal recurrence: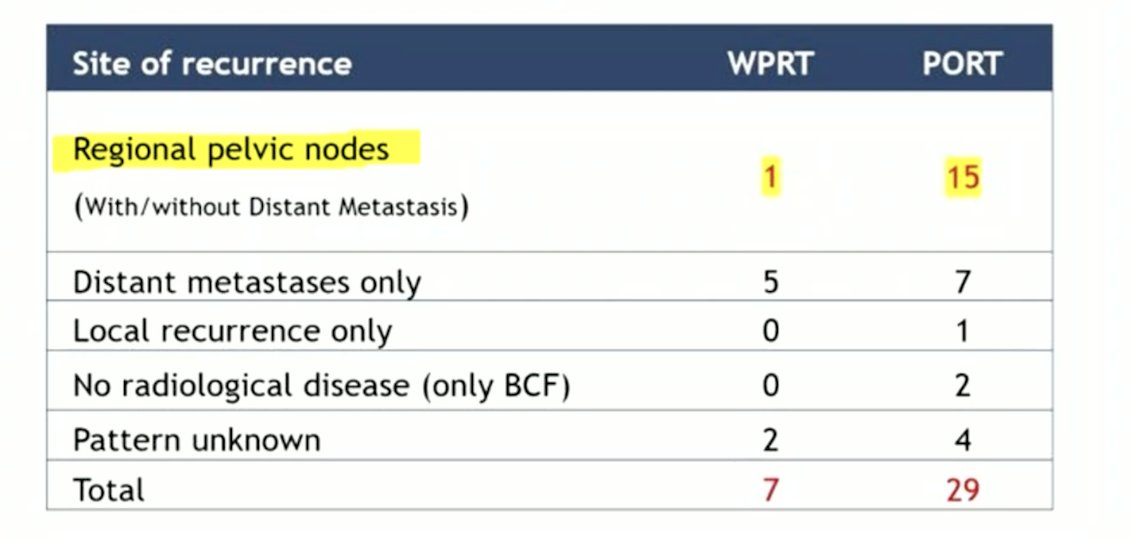
Importantly, there was no difference in patient reported quality of life outcomes for EORTC PR-25 urinary and bowel symptom domains when comparing prostate only versus whole pelvic radiotherapy: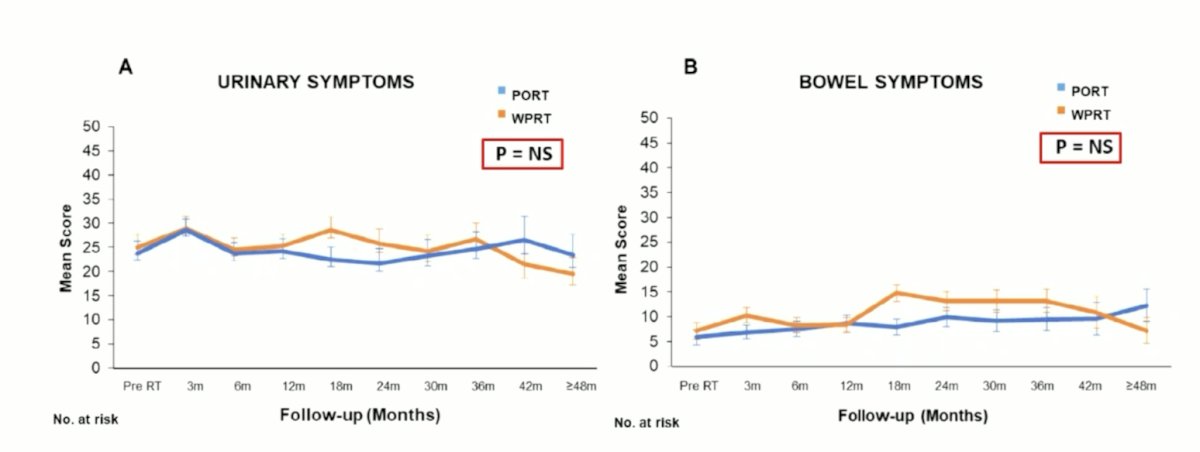
Dr. Bossi states that there is likely a sliding window of opportunity for whole pelvic radiotherapy, with the probability of metastatic disease (evaluated by PSMA PET/CT) on one side and the probability of “pure” intraprostatic disease (evaluated by the Roach formula) on the other: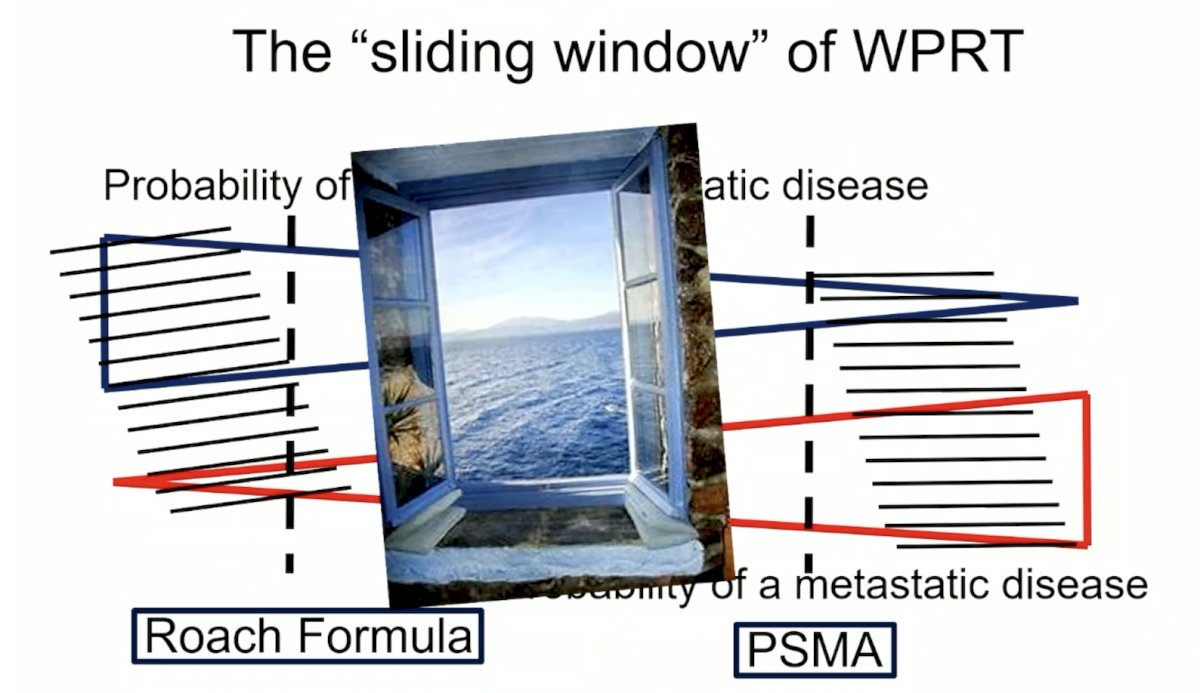
Dr. Bossi concluded his presentation discussing dose intensification and field expansion of EBRT with the following take-home points:
- For high risk patients, the EAU guidelines make several important statements:
- Treatment should not be changed based on PSMA PET/CT findings in view of the current available data
- When using PSMA PET or whole body MRI to increase sensitivity, we should be aware of the lack of outcome data on subsequent treatment change
Presented by: Alberto Bossi, MD, Gustave Roussy, Villejuif, France
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2023 European Society of Medical Oncology (ESMO) Annual Meeting, Madrid, Spain, Fri, Oct 20 – Tues, Oct 24, 2023.
References:
- Kerkmeijer LGW, Groen VH, Pos FJ, et al. Focal Boost to the Intraprostatic Tumor in External Beam Radiotherapy for Patients With Localized Prostate Cancer: Results From the FLAME Randomized Phase III Trial. J Clin Oncol. 2021;39(7):787-796.
- Kishan AU, Cook RR, Ciezki JP, et al. Radical prostatectomy, external beam radiotherapy, or External Beam Radiotherapy with Brachytherapy Boost and Disease Progression and Mortality in Patients with Gleason Score 9-10 Prostate Cancer. JAMA 2018 Mar 6;319(9):896-905.
- Murthy V, Maitre P, Kannan S, et al. Prostate-Only Versus Whole-Pelvic Radiation Therapy in High-Risk and Very High-Risk Prostate Cancer (POP-RT): Outcomes From Phase III Randomized Controlled Trial. J Clin Oncol. 2021;39(11):1234-42.


