(UroToday.com) The 2024 European Society of Medical Oncology (ESMO) Annual Congress held in Barcelona, Spain was host to the session Updates in the management of advanced renal cell carcinoma. Dr. Chad Tang posed the question of whether there is a role for radiation therapy in advanced RCC. and moved on to discuss this important topic.
Dr. Tang began his presentation by addressing the historical reasons why radiation has not been widely used for renal cell carcinoma (RCC). He explained that RCC was traditionally considered a radio-resistant neoplasm. This belief stems from a meta-analysis conducted by Deschavanne et al., which compiled radiation sensitivity data from various publications on different tumor types. However, the meta-analysis had several limitations, including the fact that only one study (n=1) specifically assessed radiation resistance in RCC. Additionally, the mean inactivating dose was low (4.80 Gy), and the surviving fraction after 2 Gy was relatively high at 0.81.1 Furthermore, Chang et al. demonstrated that a single RCC cell line (ACHN cell line) an epithelial morphology cell line isolated in 1979 from a 22-year-old male patient with metastatic papillary RCC derived from a malignant pleural effusion, was the most resistant to 2 Gy of radiation.
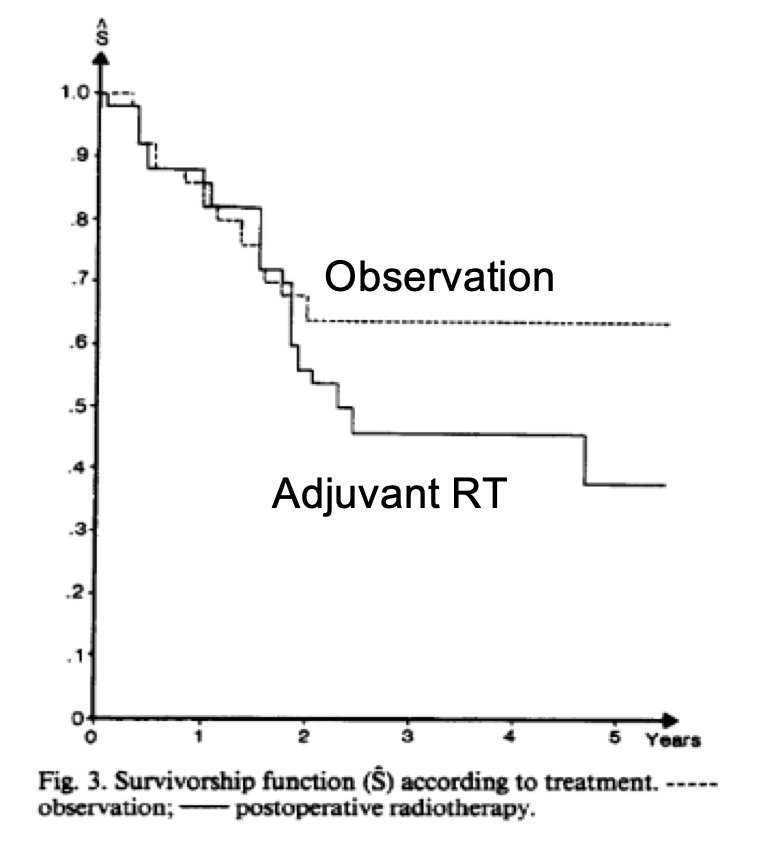
One of the last randomized trials investigating radiation therapy in RCC was published by Kjaer et al. in 1987. In this study, 65 patients with locally advanced RCC who had undergone nephrectomy were randomized to receive either radiation therapy (50 Gy in 20 fractions to the kidney bed and regional ipsilateral and contralateral lymph nodes) followed by observation, or observation alone. Unfortunately, 43% of the patients experienced relapse and died in the observation period, with no significant differences between the two groups. Additionally, several complications, mostly gastrointestinal, and five resulted in death without evidence of recurrence (19% of grade 5 toxicity). This led the study group to conclude that radiation therapy was associated with an unacceptable complication rate. As a result, the protocol was closed early after a futility analysis.2 The Kaplan-Meier graphic of survival is shown below.
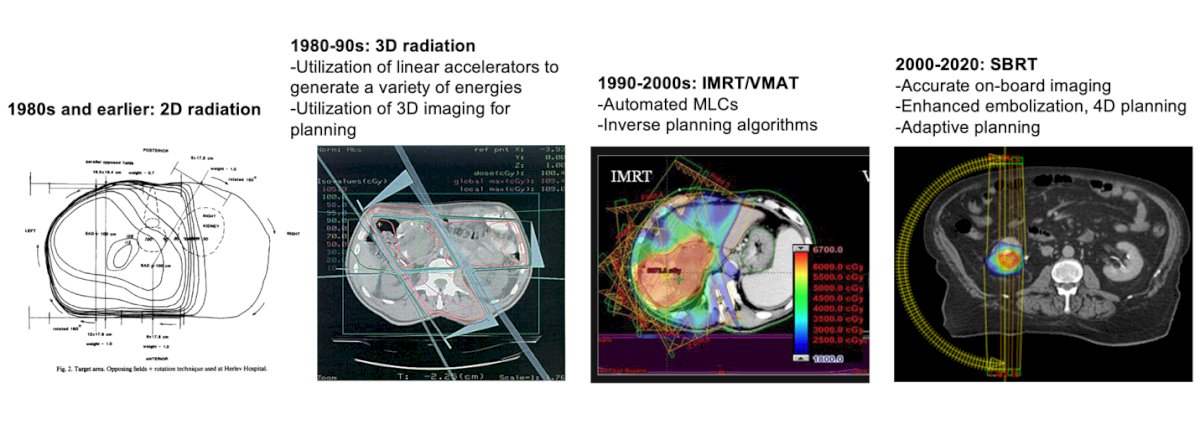
Dr. Tang discussed the significant advancements in radiation therapy over the past 30 years. He began with the 1980s, when 2D radiation was the standard, and then moved on to the 1980s-90s, when 3D imaging was introduced for planning, and linear accelerators were used to generate a variety of energies. This was followed by the development of intensity-modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT), which enabled radiation oncologists to automate multi-leaf collimators (MLCs) and use inverse planning algorithms to optimize radiation delivery and reduce toxicity. The most recent innovation, from the 2000s to the 2020s, is stereotactic body radiation therapy (SBRT), which has allowed for more accurate on-board imaging, enhanced embolization, 4D planning, and adaptive planning. These advances and innovations have completely reshaped the way we treat our patients with radiation therapy, and therefore, we should not judge radiation therapy solely based on the earlier results from the early trials.
The first attempt at metastasis-directed therapy (MDT) for metastatic RCC was presented at the American Association of Genitourinary Surgeons in 1938. In this case, a patient with RCC and a solitary pulmonary metastasis was treated with nephrectomy followed by a subtotal lobectomy, and the patient survived beyond 5 years without any evidence of disease (NED). This led to the introduction of the concept of oligometastatic RCC, which involves patients with only a limited number of metastatic sites (≤3-5). The current NCCN guidelines recommend MDT, either through metastasectomy or SBRT, for both clear cell and non-clear cell RCC.3
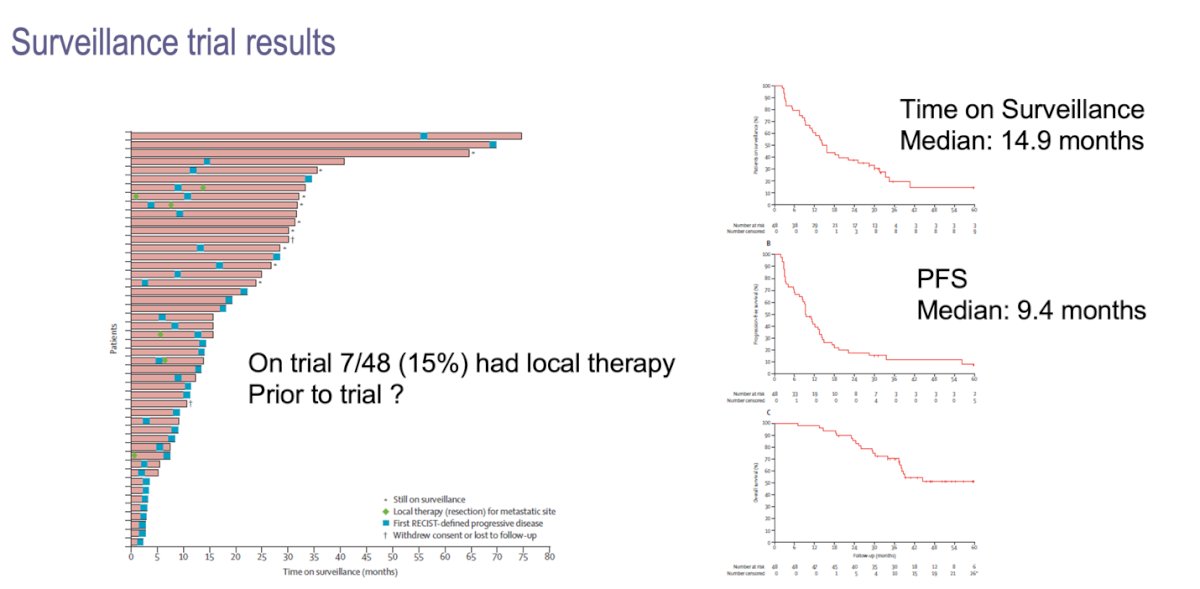
A phase 2 trial involving 48 systemic therapy-naïve metastatic RCC patients, 71% of whom had lung metastases, evaluated the management of these patients with surveillance. The primary outcome was the time until the initiation of systemic therapy (time on surveillance). Fifteen percent of the patients received local therapy prior to the trial. With a median follow-up of 38 months, the median time on surveillance was 14.9 months, and the median progression-free survival was 9.4 months (illustrated below). This study confirmed that a subset of patients with metastatic renal cell carcinoma can safely undergo surveillance before starting systemic therapy.4
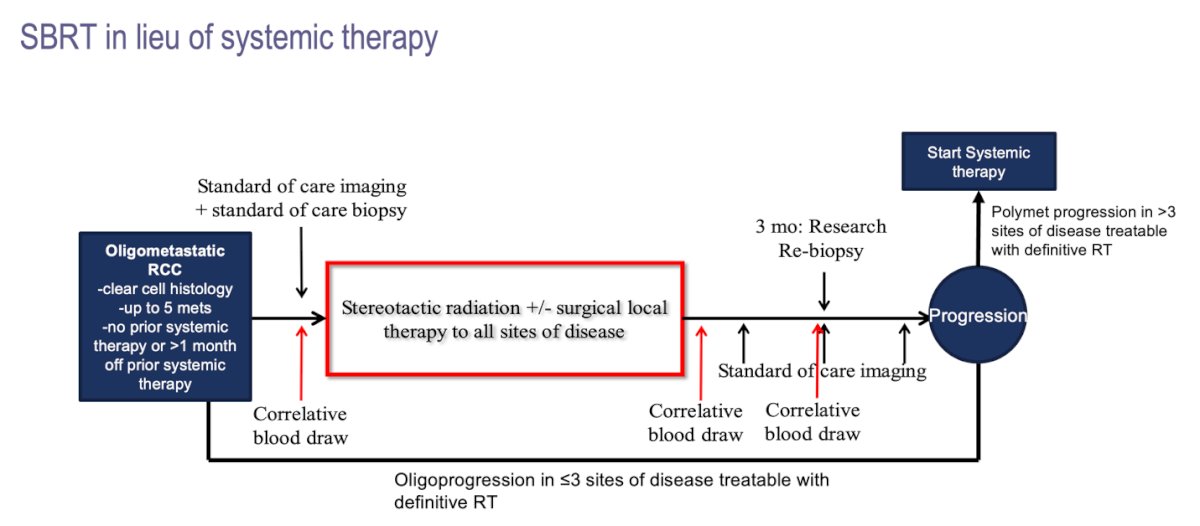
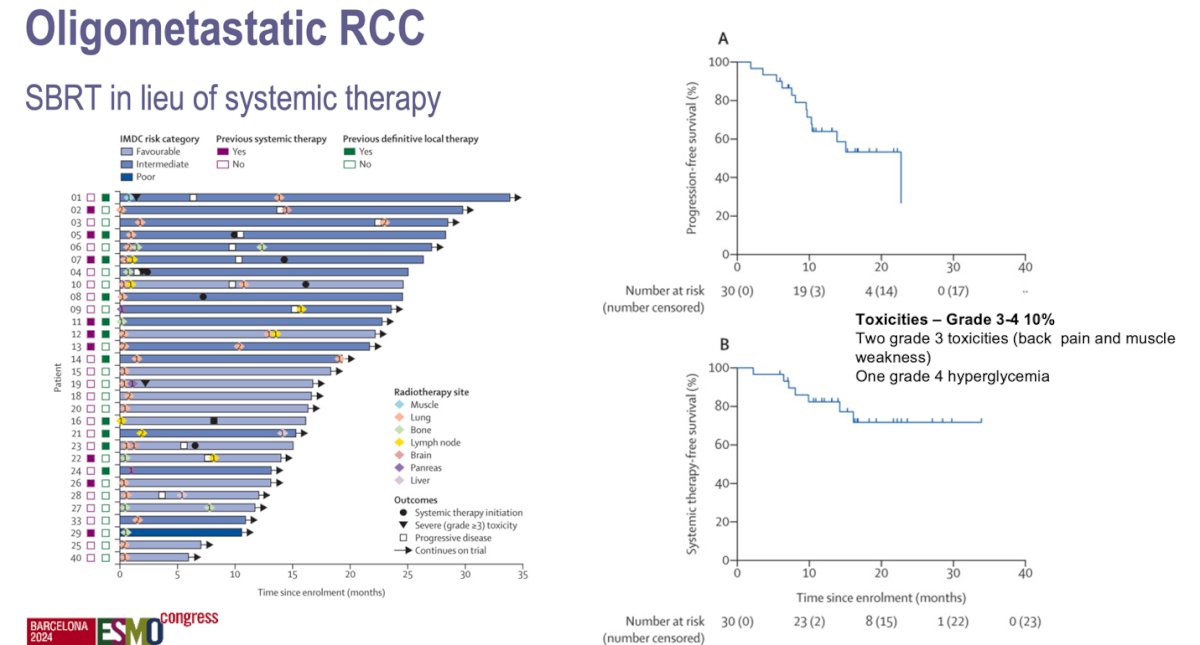
Dr. Tang presented his single-arm, single-center, phase 2 feasibility trial assessing SBRT with or without surgical local therapy to metastatic sites in patients with oligometastatic RCC (≤ 5 metastases) with clear cell histology. In this trial, patients were treated with stereotactic body radiotherapy (defined as ≤5 fractions with ≥7 Gy per fraction) to all lesions and were maintained off systemic therapy. The study flowchart is illustrated below.
Thirty patients were enrolled in this trial from 2018 to 2020. All patients had undergone nephrectomy before enrollment and completed at least one round of radiotherapy. The median progression-free survival was 22.7 months, and the one-year progression-free survival rate was 64%. Grade 3-4 toxicities were reported in 10% of patients, including two cases of grade 3 toxicity (back pain and muscle weakness) and one case of grade 4 toxicity (hyperglycemia). There were no treatment-related deaths reported by Dr. Tang.5
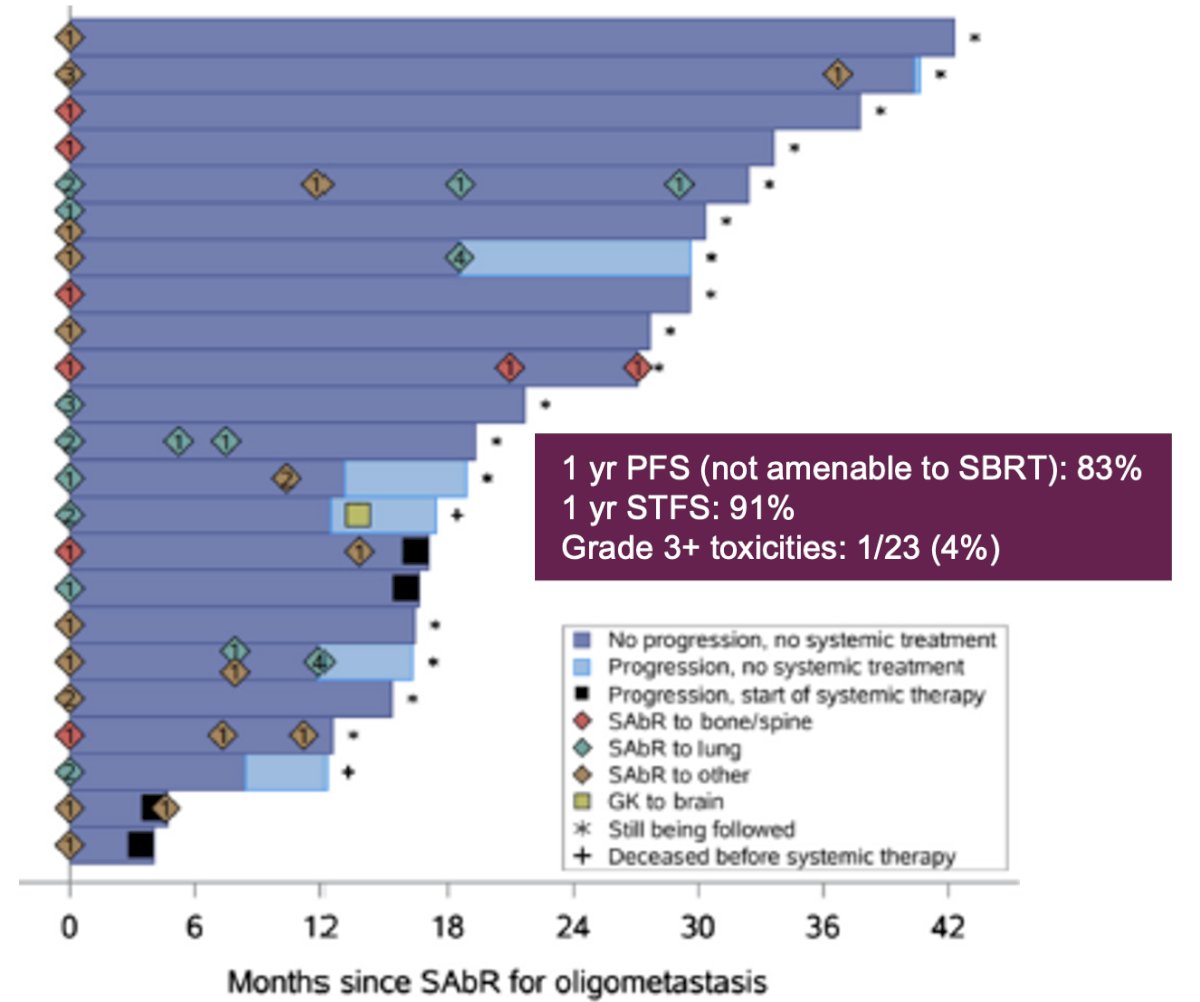
A similar phase 2 trial by Hannan et al., which included 20 patients with oligometastatic RCC receiving first- to fourth-line systemic therapy, treated oligoprogressing metastases with SBRT. The study showed a 1-year progression-free survival of 83% and a 1-year systemic therapy-free survival of 91%, with grade 3 toxicities reported in 4% of patients.6
Dr. Tang then discussed the importance of charting a path toward systemic therapy de-escalation in oligometastatic RCC, especially considering the costs and side effects associated with systemic therapy. The average cost of systemic therapy, such as IO/IO or IO/TKI doublets, ranges from $100,000 to $250,000 per year and is associated with 45-85% grade 3 toxicities. In contrast, SBRT costs approximately $20,000 to $40,000 per round and is associated with 5-20% grade 3 or higher toxicities. Furthermore, there is no evidence suggesting that patients fare worse after MDT.
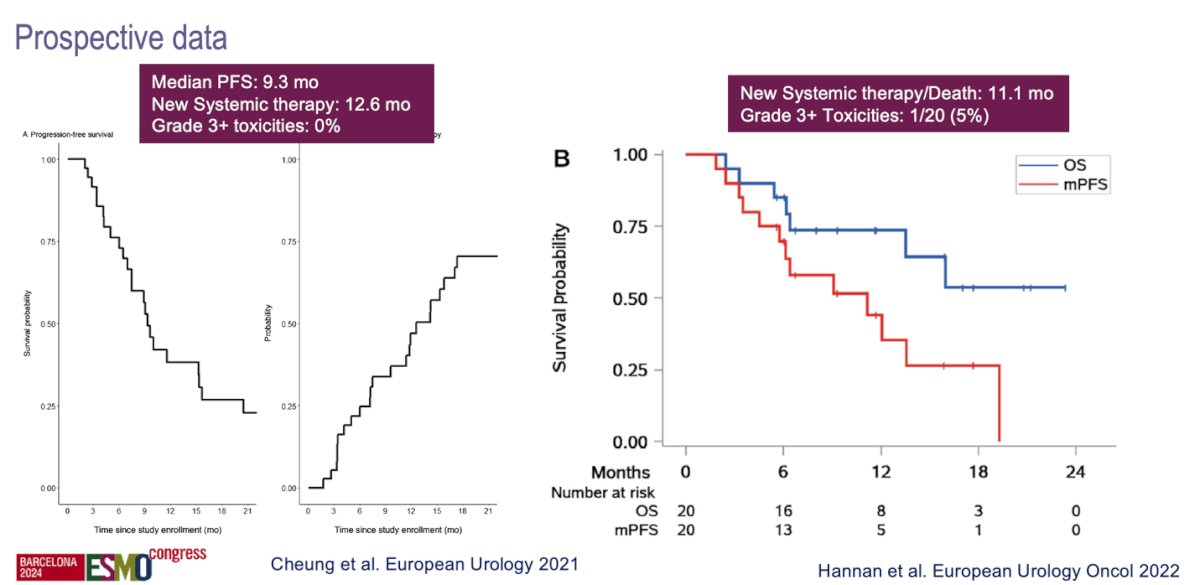
Metastasis directed therapy with systemic therapy for metastatic RCCDr. Tang then discussed the role of adding MDT to systemic therapy, introducing the concept of oligoprogression in metastatic RCC. He explained that oligoprogressive disease refers to patients who initially have an unlimited number of metastatic lesions but, through active systemic therapy, achieve control of all lesions except for a limited number of growing ones (oligoprogressive lesions). He cited prospective data from a multicenter study7 and a single centre study6 that evaluated the use of SBRT in patients with oligoprogressive RCC. These studies demonstrated that, with the addition of SBRT, systemic therapy was delayed by a median of more than one year (12.6 months)7 and 11.1 months.6
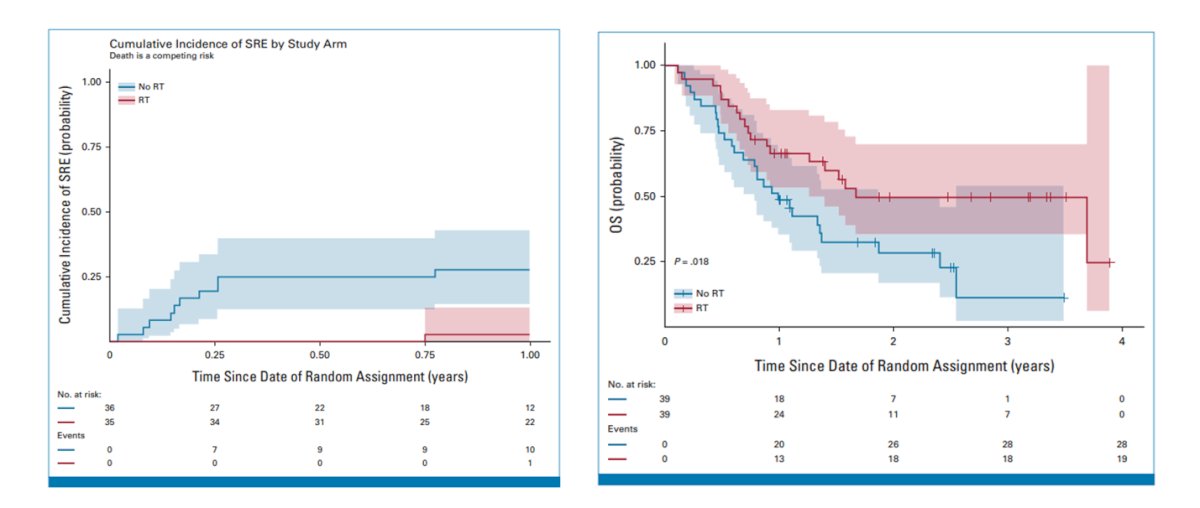
Dr. Tang presented data from a randomized clinical trial involving 78 patients with metastatic RCC who were asymptomatic and had high-risk bone metastases at more than 5 metastatic sites. The trial randomized patients to either prophylactic radiation or observation.8 See the study flowchart below.
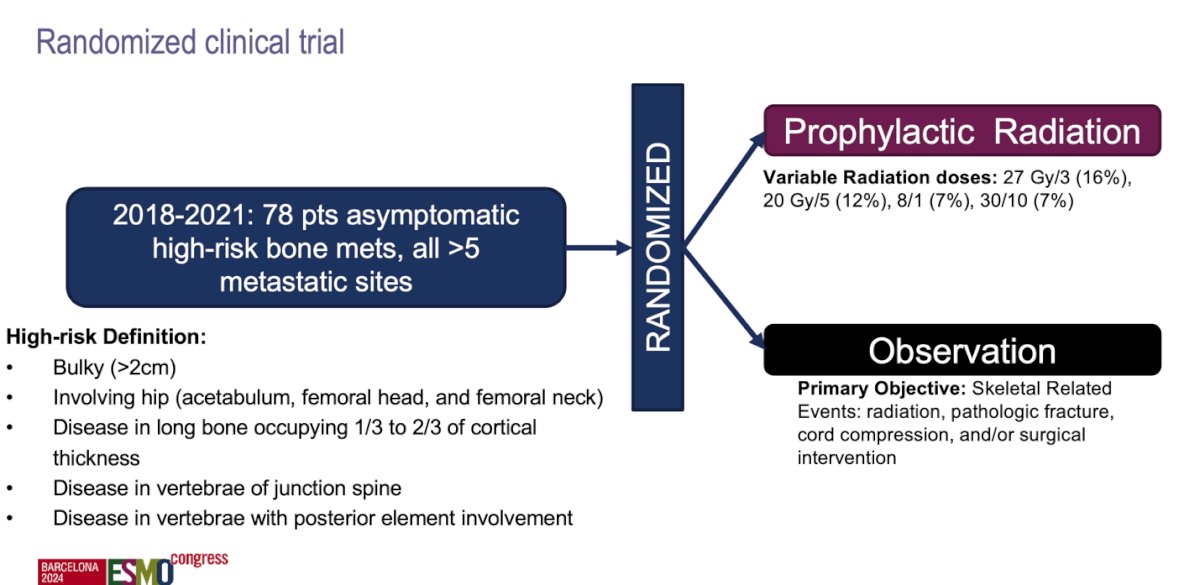
The trial found that prophylactic radiation delivered to asymptomatic, high-risk bone metastases reduced skeletal-related events and hospitalizations, and improved overall survival.
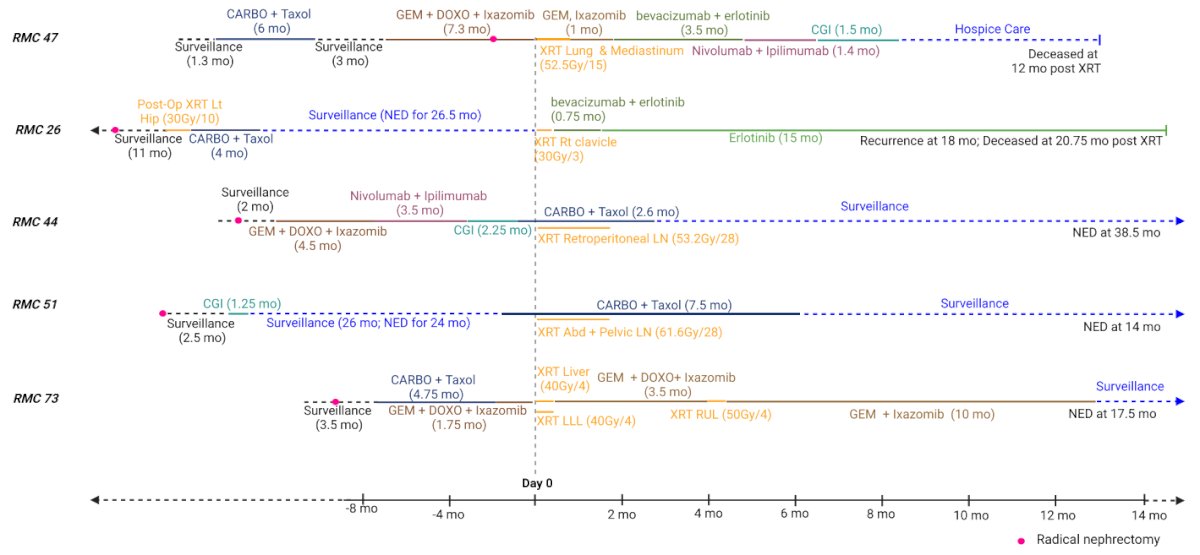
Dr. Tang also discussed the role of MDT for oligometastatic variant RCC, specifically focusing on renal medullary carcinoma. This rare and almost always fatal disease primarily affects young men and women, with a median life expectancy of just 13 months from diagnosis. Recent molecular characterization of renal medullary carcinoma has revealed SNARCB1 mutations that lead to high MYC expression, which may sensitize these tumor cells to PARP inhibitors. This represents an intriguing potential target for exploration in these patients.9 He showed ta study treating patients with renal medullary carcinoma with combination of chemotherapy, immunotherapy, and radiation therapy to metastatic sites with 3/5 patients rendered NED and stopping systemic treatment without recurrence.10
Dr Tang concluded his presentation with the following remarks:
- Historically, radiation was not used for RCC due to in vitro data showing radioresistance in a single RCC cell line and early randomized trials that found no benefit and significant toxicities with adjuvant radiation.
- Targeting and radiation therapy have significantly advanced over the last 30 years.
- Two prospective trials have demonstrated that radiation can potentially defer systemic therapy for over one year.
- MDT-based approaches are generally less toxic, less expensive, and require fewer hospital visits compared to systemic therapy. However, randomized phase III data is still needed.
- For oligoprogression, two prospective trials have shown the potential to delay escalation of systemic therapy for approximately one year.
- Prophylactic radiation for high-risk bone metastases may prevent serious skeletal-related events, which could impact morbidity and mortality, especially as patients live longer.
- Renal medullary carcinoma appears to be sensitive to radiation and consolidation of disease in heavily pre-treated patients has been associated with durable remissions.
Presented by: Chad Tang, MD, Department of Radiation Oncology, MD Anderson Cancer Center, Houston, TX.
Written by: Julian Chavarriaga, MD – Urologic Oncologist at Cancer Treatment and Research Center (CTIC) Luis Carlos Sarmiento Angulo Foundation via Society of Urologic Oncology (SUO) Fellow at The University of Toronto. @chavarriagaj on Twitter during the 2024 European Society of Medical Oncology (ESMO) Annual Meeting, Barcelona, Spain, Fri, Sept 13 – Tues, Sept 17, 2024.
References:- Deschavanne, Patrick J., and Bernard Fertil. "A review of human cell radiosensitivity in vitro." International Journal of Radiation Oncology* Biology* Physics 34.1 (1996): 251-266.
- Kjaer, Mogens, Peter L. Frederiksen, and Svendrage Engelholm. "Postoperative radiotherapy in stage II and III renal adenocarcinoma. A randomized trial by the Copenhagen Renal Cancer Study Group." International Journal of Radiation Oncology* Biology* Physics 13.5 (1987): 665-672.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Guideline Kidney Cancer V.1.2025. © National Comprehensive Cancer Network, Inc. 202X. All rights reserved. Accessed [September 14, 2024]. To view the most recent and complete version of the guideline, go online to NCCN.org.
- Rini, Brian I., et al. "Active surveillance in metastatic renal-cell carcinoma: a prospective, phase 2 trial." The Lancet Oncology17.9 (2016): 1317-1324.
- Tang, Chad, et al. "Definitive radiotherapy in lieu of systemic therapy for oligometastatic renal cell carcinoma: a single-arm, single-centre, feasibility, phase 2 trial." The lancet oncology22.12 (2021): 1732-1739.
- Hannan, Raquibul, et al. "Phase II trial of stereotactic ablative radiation for oligoprogressive metastatic kidney cancer." European urology oncology 5.2 (2022): 216-224.
- Cheung, Patrick, et al. "Stereotactic radiotherapy for oligoprogression in metastatic renal cell cancer patients receiving tyrosine kinase inhibitor therapy: a phase 2 prospective multicenter study." European Urology 80.6 (2021): 693-700.
- Gillespie, Erin F., et al. "Prophylactic radiation therapy versus standard of care for patients with high-risk asymptomatic bone metastases: a multicenter, randomized phase II clinical trial." Journal of Clinical Oncology 42.1 (2024): 38-46.
- Msaouel, Pavlos, et al. "Comprehensive molecular characterization identifies distinct genomic and immune hallmarks of renal medullary carcinoma." Cancer Cell 37.5 (2020): 720-734.
- Mbilinyi, Robert H., et al. "Radiation Therapy for the Management of Renal Medullary Carcinoma: A Multi-Case Study." Clinical Genitourinary Cancer 22.3 (2024): 102065.