Dr. Shariat began by arguing that the adoption of new technologies should be driven by superior or equivalent: cancer outcomes; quality of life; perioperative functional outcomes, blood loss, operative time, complications, length of stay; and costs.
In the context of radical nephroureterectomy, Dr. Shahrokh Shariat showed data demonstrating that both open and laparoscopic radical nephroureterectomy is decreasing with robotic approaches supplanting both. This was particularly true among patients with high-grade pathology.
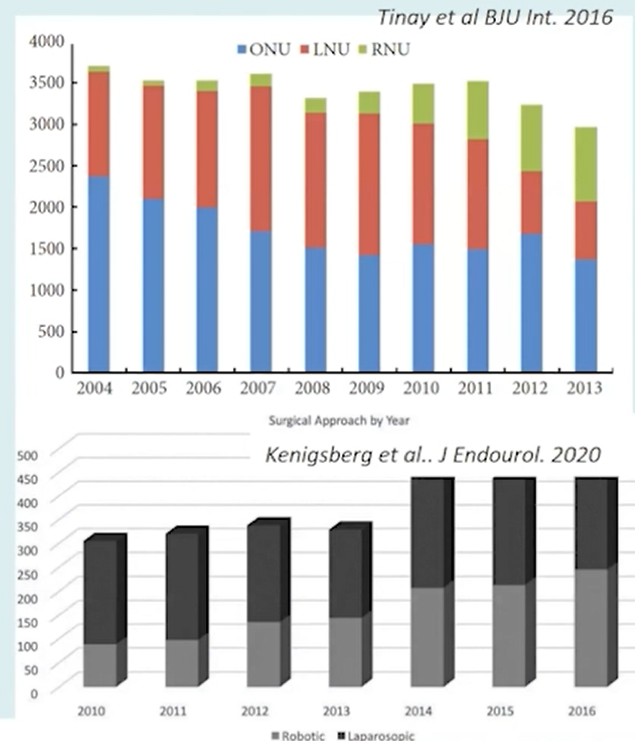
From 2010 to 2016, the proportion of cases approaches robotically has nearly doubled from 29 to 56% in the United States.
Moving back in time, Dr. Shariat examined data comparing laparoscopic and open radical nephroureterectomy, emphasizing the importance of precautions with pneumoperitoneum to avoid spillage including avoiding entering the urinary tract, avoiding direct contact between the instruments and tumors, using a closed system with specimen extraction via endobag, and removal of the kidney and ureter en bloc with a bladder cuff. Further, guidelines recommend caution with the use of minimally invasive approaches for patients with advanced disease.
He then highlighted Simone and colleagues who published a randomized comparison of open and laparoscopic radical nephroureterectomy among 80 patients, demonstrating worse outcomes among those with pT3 or high-grade disease treated minimally invasively. Further, a systematic review demonstrated that oncologic outcomes of laparoscopic approaches may be poorer than open when the bladder cuff is approached laparoscopically (leading to increased rates of bladder recurrence) and in patients with locally advanced, high-risk disease.
Dr. Shariat described the many techniques proposed for minimally invasive management of the distal ureter, highlighting data showing that, for example, stapling across the ureter was associated with higher rates of recurrence. A further systematic review and meta-analysis demonstrated that a laparoscopic approach was associated with an increased risk of intravesical recurrence. Further, the transition to laparoscopic approaches was associated with decreased performance of lymphadenectomy and decreased nodal yield when performed.
Dr. Shariat then highlighted that robotic approaches can potentially overcome the challenges of the laparoscopic approach which may improve the quality and utilization of lymph node dissection, improve bladder cuff dissection leading to lower positive surgical margins, and less conversion.
Considering the initial criteria for adoption of new approaches, Dr. Shariat emphasized that, based on a recently published meta-analysis, surgical approach (open versus robotic) is not associated with short term differences in recurrence-free or cancer-specific survival, though these conclusions should be tempered by the overall low quality of data and few patients included.
In terms of quality of life, patients have lower perioperative analgesia requirements but longer-term outcomes, in Dr. Shariat’s view, likely do not differ. In terms of other perioperative functional outcomes, prior systematic reviews of more than 85,000 patients have demonstrated lower blood loss and transfusion rates for patients treated robotically while operative times have been reported to be shorter with an open approach through the newer robotic platforms which do no require redocking may shift this balance. Further, robotic approaches are associated with shorter hospital stays. However, robotic surgery was associated with higher readmission rates, without any meaningful differences in complication rates.
In terms of cost, robotic approaches are more expensive, in particular, due to supply-related costs though this may differ between health systems.
Considering the question of whether to favour an open or robotic approach for high-risk UTUC, Dr. Shariat posited that open should be the preferred approach for patients in which non-organ confined disease is expected until proven otherwise.
In closing, he highlighted that adoption of the robotic approach has had similar outcomes across urologic disease, without meaningful differences in long-term outcomes.

Presented by: Shahrokh F. Shariat, MD, Medical University of Vienna, Vienna, Austria
Written by: Christopher J.D. Wallis, MD, PhD, FRCSC Contact: @WallisCJD on Twitter during the 18th Meeting of the EAU Section of Oncological Urology (ESOU21), January 29-31, 2021


