In the spring of 2020, at the onset of the pandemic, Wallis and colleagues provided a multi-disciplinary approach to recommendations for aiding in the triage and management during the COVID-19 pandemic:1
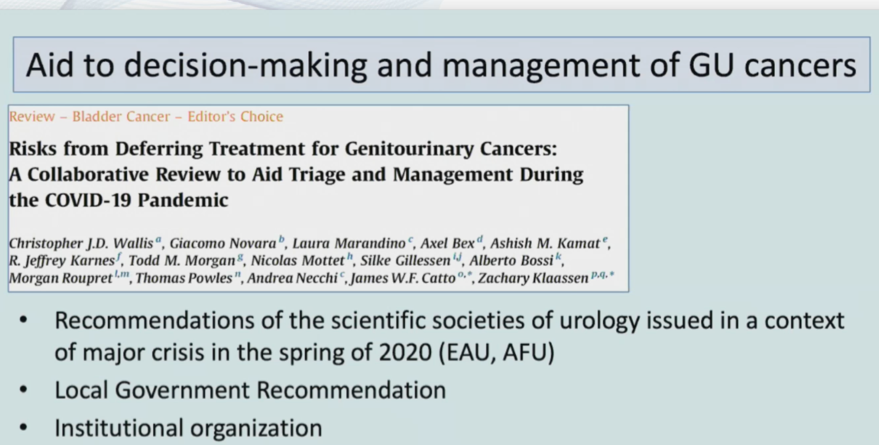
The following points provided by Dr. Lenfant highlight the recommendations from this paper.
Bladder Cancer:
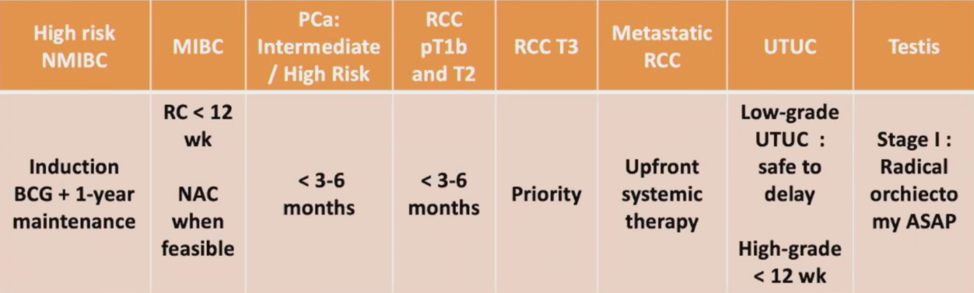
- Low-grade NMIBC: it is safe to defer cystoscopic surveillance and transurethral resection of bladder tumor for recurrence in patients with known low-grade disease
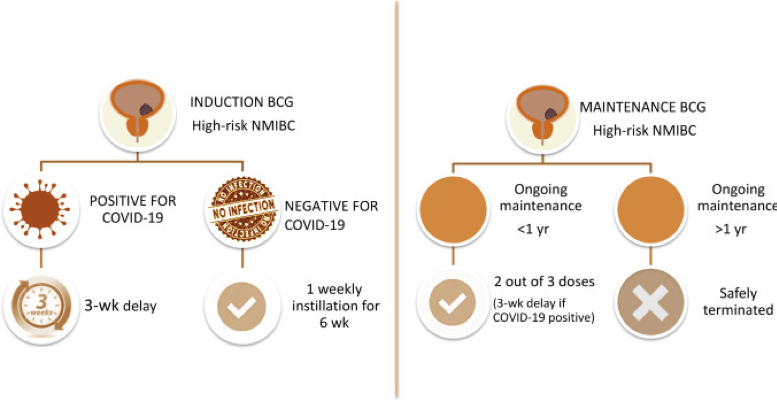
- High-grade NMIBC: an induction and one course of maintenance therapy (6+3) should be offered as first-line therapy. Dr. Lenfant was also the lead author on the following recommendations for delivering BCG during the COVID-19 pandemic:2
- Muscle-invasive bladder cancer: delays in radical cystectomy of up to 12 weeks may be safe, and neoadjuvant chemotherapy should be considered when feasible. Ultimately, clinicians should prioritize radical cystectomy over other urologic oncology procedures during the COVID-19 restrictions
- Low risk, localized: a delay of several months or years is unlikely to affect treatment outcomes
- Intermediate/high risk, localized: delays of 3-6 months from diagnosis does not appear to be associated with adverse pathologic outcomes, biochemical recurrence, or survival outcomes
- Small renal masses <4cm: there is robust data supporting active surveillance for masses <4 cm, even up to five years after initial diagnosis
- cT1b-T2: delays of 3-6 months do not appear to affect outcomes adversely
- >=T3: there are no studies assessing the impact of delayed surgical intervention among patients with locally advanced kidney cancer and these patients should be prioritized for surgical intervention
- Metastatic disease: upfront systemic therapy should be prioritized over cytoreductive nephrectomy in asymptomatic patients, and nephrectomy should be reserved for symptomatic patients
- Low-grade: often managed with nephron-sparing approaches and thus are likely to have a minimal risk with a surgical delay
- High-grade: delays of up to 12 weeks may not be associated with changes in survival, despite worse pathologic outcomes
- Stage I: radical orchiectomy should be performed ASAP and active surveillance should be utilized rather than preventative therapy
- Metastatic disease: there is insufficient data to provide guidance on the effects of delaying post-chemotherapy RPLND
Presented by: Louis Lenfant, Hopital Pitie-Salpetriere, Sorbonne University, Paris, France
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md during the 18th Meeting of the EAU Section of Oncological Urology (ESOU21), January 29-31, 2021
References:
- Wallis CJD, Novara G, Marandino L, et al. Risks from deferring treatment for genitourinary cancers: A collaborative review to aid triage and management during the COVID-19 pandemic. Eur Urol. 2020 Jul;78(1):29-42.
- Lenfant L, Seisen T, Loriot Y, et al. Adjustments in the use of intravesicular instillations of Bacillus Calmette-Guerin for high-risk non-muscle-invasive bladder cancer during the COVID-19 pandemic. Eur Urol 202 Jul;78(1):1-3.


