Dr. Heidegger began with a case presentation, describing a 65-year man without notable medical history. He has a family history notable for an uncle diagnosed with metastatic prostate cancer at age 57. In 2000, he underwent a transrectal ultrasound-guided biopsy which was negative, at which time his PSA was 2.9 ng/mL and his free/total ratio was 13%. Seen September 2020, the patients had a PSA of 6.2 ng/mL with a free/total ratio of 13% and a prostate specific antigen (PSA) velocity of 3.36. His digital rectal exam was unremarkable. His PHI was 63 and prostate volume was 25ccm. On multi-parametric MRI, he had a PIRADS 2 lesion. The patient underwent a repeat transrectal biopsy with both systematic and targeted cores. As a result, he was diagnosed with prostate cancer in 9 of 15 cores, with a Gleason score of 3+4 with <10% of pattern 4 for an overall ISUP grade group 2 disease.
The patient was offered surgery, radiotherapy with short-term androgen deprivation, or active surveillance. The patient underwent radical prostatectomy with pelvic lymphadenectomy. Final pathology demonstrated pT2c ISUP 2 prostate cancer with negative margins and uninvolved lymph nodes. He had an undetectable post-operative PSA and was continent at 6 weeks.
Dr. Van Den Bergh then discussed the role of surveillance in this patient’s clinical scenario. He highlighted notable features in the presentation including a PSA density of 0.25, the relatively high number of involved cores, the presence of Gleason 7 disease, and the focal cribriform histology. In spite of these, there are a number of features that speak towards more conservative approaches including the non-palpable disease, essentially benign mpMRI, and low volume of pattern 4 disease. Thus, he posed the question, “are we looking for reasons to treat or reasons to initially defer treatment?”.
He then highlighted classic data from Drs. Lu-Yao and Albertsen demonstrated that, at 15 years, the risk of other cause mortality exceeds the risk of prostate cancer mortality by a factor of 10 among men with cT1c, intermediate grade disease managed conservatively. Further, looking at the PROTECT study, he showed data that there is no difference in mortality between monitoring and active treatments. Examining subgroup analyses from PIVOT, Dr. Van Den Burgh highlighted that benefit from intervention is not clearly beneficial in this patient given the discordance between characteristics including age, comorbidity, number of cores, and disease risk categorization. He then highlighted some data from Dr. Vickers who utilized the SPCG-4 cohort to examine which patients benefited from intervention. As highlighted in the figure, this was strongly influenced by patient age. Increasing Gleason score was also associated with the magnitude of benefit.
Dr. Van Den Bergh then highlighted data from ERSPC demonstrating that the presence of cribriform growth in Gleason 7 disease was strongly predictive of outcomes, with outcomes similar to those for patients with Gleason 6 disease if no cribriform pattern was present. While the importance of this has been reiterated in consensus statements, inter-observer agreement for cribriform growth and percent pattern 4 involvement is only moderate (alpha 0.5).
Further, Dr. Van Den Bergh highlighted data from Dr. Ploussard demonstrating that outcomes, following prostatectomy, were better for patients evaluated with systematic and targeted biopsy as compared to those who received systematic biopsies alone. In contrast, he emphasized data from Dr. Klotz showing that the presence of Gleason 3+4 disease at the time of diagnosis was associated with an increased risk of metastasis while on surveillance. However, given changes in evaluation and pathological reading, currently diagnosed Gleason 3+4 may not be comparable to classic diagnoses.
Dr. Van Den Burgh presented data from Dr. Gandaglia and the YAU group examining predictors of adverse pathology at the time of radical prostatectomy. These include PSA, clinical stage, biopsy grade group, number of cores, and PSA density.
In the current clinical case, these are somewhat mixed in how we should interpret the suitability of surveillance. Further, MRI data may complement these variables. He emphasized data from Dr. Moore showing that outcomes for patients with Gleason 3+4 who do not have visible lesions on MRI are comparable to those with Gleason 3+3 and a visible lesion.
He emphasized the value of risk models to decide on the suitability for active surveillance, in order to optimize decision making. Doing so increases the pool of men potentially eligible for active surveillance. Concluding, Dr. Van Den Burgh emphasized that initial active surveillance is unlikely to cause any harm and may offer some benefit.
Dr. Hamdy then presented the data supporting active intervention. Dr. Hamdy began by highlighting the information that will be actionable and important for the patient:
Based on the patient’s characteristics, his age makes him borderline for a benefit from screening or treatment in Dr. Hamdy’s estimation while his good health increases both the potential benefit of treatment due to longer life expectancy and also the number of treatments available. His family history increases somewhat his risk of clinically significant disease while his prior work-up, from 2000, was inadequate by contemporary standards.
Dr. Hamdy emphasized that, while MRI is valuable, there is a 5-15% risk of missing significant cancer with a PIRADS2 lesion. In terms of the diagnostic approach, Dr. Hamdy emphasized that targeted biopsy of PIRADS2 lesions is not widespread. Further, transrectal approaches may be superseded in the future by transperineal approaches.
Dr. Hamdy then emphasized that, based on the history, one may assume that the patient likely had prostate cancer 20 years prior that was not detected based on the biopsy performed and has thus been on very “inactive” surveillance for 20 years.
Dr. Hamdy highlighted that evidence for therapeutic options, based on data from PROTECT, showed that disease-specific (1%) and all-cause mortality (10%) were relatively low regardless of treatment approach, however, there was a 50% reduction in progression/metastases with radical treatment.
Considering treatment choices, it is important to consider the side effects of treatment, in addition to efficacy outcomes. Again, he emphasized data from the PROTECT cohort.
In the context of the case, Dr. Hamdy emphasized that there are a number of unfavorable features including family history, tumor volume (number of cores involved), and the presence of Gleason pattern 4 and cribriform disease. In terms of treatment approach, Dr. Hamdy wondered as to the value of node dissection in this case, as well as the relatively low yield for an extended dissection.
Dr. Hamdy addressed the question of whether he would offer active treatment, answering in the affirmative, as one of the options including surgery, radiotherapy approaches, and surveillance, with a discussion of oncologic and functional outcomes.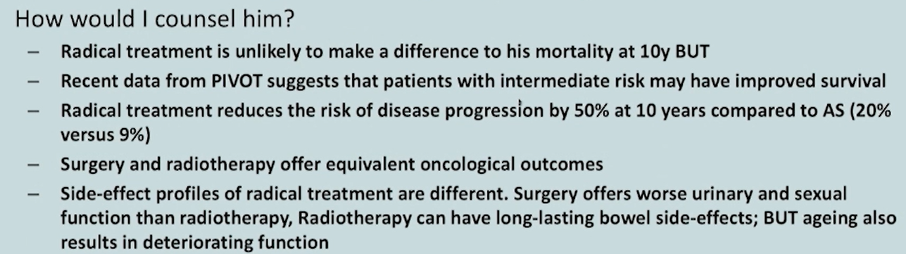
In terms of a final decision, he emphasized that there are trade-offs that must be balanced on the basis of a patient and their partner’s priorities.
Presented by: Isabel Heidegger, Dr, PhD, FEBU, Associate Professor, Department of Urology, Medical University Innsbruck, Innsbruck, Austria, Freddie Hamdy, MBChB, LRCSPEd, LRCSEd, LRCPSGlasg, FRCSEd, MD, FRCSEd(Urol), MA (Oxon), FRCS, FMedSci., Nuffield Professor of Surgery, Professor of Urology, University of Oxford, Oxford, UK, and Roderick Van Den Bergh, MD, Urologist at St. Antonius Ziekenhuis, Carlton North, Victoria, Australia
Written by: Christopher J.D. Wallis, MD, Ph.D., FRCSC, Instructor in Urology, Vanderbilt University Medical Center, Nashville, Tennessee @WallisCJD on Twitter during the 18th Meeting of the EAU Section of Oncological Urology (ESOU21), January 29-31, 2021


