(UroToday.com) At the 2021 European Association of Urology (EAU) Section of Oncological Urology (ESOU) Virtual Annual Meeting, the EAU Section of Urological Research (ESUR) lecture was provided by Dr. Karen Knudsen discussing when and how to provide genetic testing for prostate cancer. Dr. Knudsen pointed out that there is an extraordinary burden of prostate cancer in the US, ranked as #1 for males in estimated new cases and #2 in estimated cancer-related deaths. Germline testing is revolutionizing care, with 12-17% of metastatic patients having germline mutations and 5-7% of early-stage patients having germline mutations. As such, germline testing is impacting precision medicine and tailored screening approaches, which also has an impact on families for hereditary cancer risk.
Dr. Knudsen, who works at the Sidney Kimmel Cancer Center in Philadelphia, Pennsylvania, notes that there is an extraordinary burden of prostate cancer seen at her institution. In fact, Philadelphia outpaces the state and the US in prostate cancer incidence and mortality: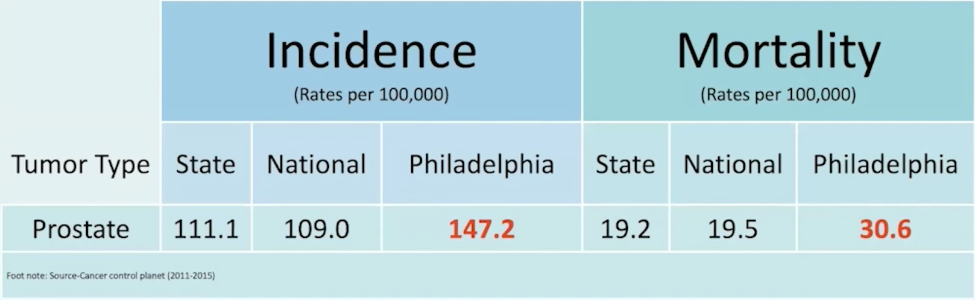
In the Philadelphia area, thousands of men and families need access to genetic counseling and genetic testing in order to reduce prostate cancer mortality. According to Dr. Knudsen, there are several reasons for this disparity in the Philadelphia area, including (i) having a high incidence of smoking (a top 10 city) and tobacco-related cancers, (ii) obesity rates far exceed national averages secondary to poor nutrition, and (iii) a lack of transportation with 16% of patients at her institution without sufficient travel arrangements.
The Sidney Kimmel Cancer Center’s men’s genetic risk clinic is led by Dr. Veda Giri. In terms of genetic counseling and testing, patients are seen across a 3-stage geographic landscape, with five genetic counselors providing care across the Jefferson Health System; during the pandemic, 95% of visits were via telehealth. Genetic case conference discussions occur on a weekly basis with the entire team, with over 3,000 cases in their database since 2015. The Sidney Kimmel Cancer Center model is as follows:
The result of this approach has led to the Philadelphia Consensus Conference, which has been influential in spearheading national guidelines, including “Role of Genetic Testing for Inherited Prostate Cancer Risk: Philadelphia Prostate Cancer Consensus Conference 2017”1 and “Implementation of Germline Testing for Prostate Cancer: Philadelphia Prostate Cancer Consensus Conference 2019”.2
The National Comprehensive Cancer Network (NCCN) Guidelines Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic (Version 1.2021) and NCCN Guidelines Prostate Cancer Version (2.2020) recommend germline testing in the following patient groups:
- Metastatic prostate cancer
- Ashkenazi Jewish ancestry
- Intraductal/cribriform histology
- Very high-risk disease: T3b-T4 or primary Gleason pattern 5 or >4 cores with Grade Group 4/5
- High-risk disease: T3a or Grade Group 4 or 5 or PSA >20
One of the issues with germline testing is the variability in multigene panels for testing:2
As follows is an important table highlighting the clinical implications of germline testing for prostate cancer:
Dr. Knudsen provided the following conclusions from her presentation discussing germline mutation testing for patients with prostate cancer:
- Germline testing is now central to prostate cancer treatment, risk assessment, and hereditary cancer evaluation. This is likely to have a future impact on early-stage disease management
- Close collaboration is needed between cancer genetics, urology, and oncology to streamline genetic evaluation strategies
- There are multiple areas that require attention, including disparities in genetic knowledge and engagement in genetic testing, healthcare provider education, implementation across practice settings, advocacy and policy changes to make germline testing accessible, and increased population awareness
Written by: Zachary Klaassen, MD, MSc, Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md during the 18th Meeting of the EAU Section of Oncological Urology (ESOU21), January 29-31, 2021
References:
1. Giri, Veda N., Karen E. Knudsen, William K. Kelly, Wassim Abida, Gerald L. Andriole, Chris H. Bangma, Justin E. Bekelman et al. "Role of genetic testing for inherited prostate cancer risk: Philadelphia Prostate Cancer Consensus Conference 2017." Journal of Clinical Oncology 36, no. 4 (2018): 414.
2. Giri, Veda N., Karen E. Knudsen, William K. Kelly, Heather H. Cheng, Kathleen A. Cooney, Michael S. Cookson, William Dahut et al. "Implementation of germline testing for prostate cancer: Philadelphia prostate cancer consensus conference 2019." Journal of clinical oncology: official journal of the American Society of Clinical Oncology 38, no. 24 (2020): 2798-2811.


