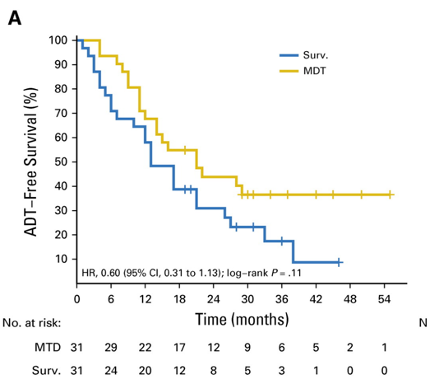
In the STOMP trial1, Ost and colleagues randomly assigned 62 patients to either surveillance or metastasis-directed therapy of all detected lesions (surgery or stereotactic body radiotherapy), with a primary end point of androgen deprivation therapy (ADT)-free survival. At a median follow-up time of 3 years (IQR 2.3-3.75 years), the median ADT-free survival was 13 months (80% confidence interval [CI] 12 to 17 months) for the surveillance group and 21 months (80% CI 14 to 29 months) for the metastasis-directed therapy group (hazard ratio [HR] 0.60, 80% CI 0.40 to 0.90; log-rank p = 0.11):
Dr. De Meerleer notes that the difficulty with a randomized controlled trial evaluating stereotactic body radiation therapy +/- systemic treatment is that it is difficult to appropriately delineate the control group (ADT versus androgen receptor-targeted agent), as well as implications for cost, toxicity, and how long to continue treatment:
The Phase II ORIOLE trial2 randomized 54 men in a 2:1 ratio to receive stereotactic body radiotherapy or observation. The primary endpoint for this trial was progression at 6 months, defined as a prostate-specific antigen (PSA) increase, radiographic or symptomatic progression, ADT initiation, or death. Progression at 6 months occurred in 7 of 36 patients (19%) receiving stereotactic body radiotherapy and 11 of 18 patients (61%) undergoing observation (p = 0.005). Furthermore, treatment with stereotactic body radiotherapy improved median progression-free survival (not reached vs. 5.8 months; HR 0.30, 95% CI 0.11-0.81; p = 0.002):

For those patients in the stereotactic body radiotherapy arm that had a prostate-specific membrane antigen (PSMA) PET-CT scan, the proportion of men with disease progression at 6 months was 5% in those who did not have any untreated lesions compared to 38% in those who did have some untreated PSMA avid lesions (p=0.03). Dr. De Meerleer notes that the optimal randomized controlled trial should use PSMA PET-CT and not conventional imaging for assessing eligibility criteria.
In an analysis comparing the impact of 18F-fluorocholine and gallium-68PSMA PET-CT-guided metastases-directed therapies in patients with castration-sensitive oligorecurrent prostate cancer, Mazzola et al.3 assessed a total of 118 lesions in 88 patients. The median pre-stereotactic body radiation therapy PSA was 2.04 ng/mL in the 18F-fluorocholine PET cohort and 0.58 ng/mL in the 68PSMA PET-CT arm. Disease-free survival rates were 63.6% and 34%, respectively, in the 68PSMA PET-CT and 18F-fluorocholine PET-CT (p = 0.06). Furthermore, the ADT administration rate was higher after 18F-fluorocholine PET-CT stereotactic body radiation therapy (SBRT) (p = 0.001) owing to the higher incidence of polymetastatic disease after first-course SBRT compared with 68PSMA PET-CT arm:
Finally, Dr. De Meerleer discussed the Phase III trial comparing single-dose 24 Gy radiotherapy to a 3-fraction stereotactic body radiation therapy regimen in the treatment of oligometastatic cancer.4 Between November 2010 and September 2015, 117 patients with 154 oligometastatic lesions (≤ 5/patient) were randomized in a 1:1 ratio to receive 24 Gy ultra-high single-dose radiotherapy or 3 x 9 Gy stereotactic body radiation therapy. There were 59 patients with 77 lesions that were randomized to 24 Gy ultra-high single-dose radiotherapy and 58 patients with 77 lesions to 3 x 9 Gy stereotactic body radiation therapy. The cumulative incidence of local recurrence for ultra-high single-dose radiotherapy lesions was 2.7% (95% CI 0-6.5%) and 5.8% (95% CI 0.2-11.5%) at years two and three, respectively. This is in comparison to 9.1% (95% CI 2.6-15.6%) and 22% (95% CI 11.9-32.1%) for stereotactic body radiation therapy lesions (p =0.0048). As such, it is important to keep an open mind to additional approaches to the delivery of therapy, for example in this case where ultra-high single-dose radiotherapy was reported as a superior ablative treatment to stereotactic body radiation therapy for patients with oligometastatic lesions.
Presented by: Gert De Meerleer, MD, PhD, Department of Radiation Oncology, University Hospitals Leuven, Leuven, Belgium
Written by: Zachary Klaassen, MD, MSc, Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, Georgia, Twitter: @zklaassen_md during the 18th Meeting of the EAU Section of Oncological Urology (ESOU21), January 29-31, 2021
References:
1. Ost, Piet, Dries Reynders, Karel Decaestecker, Valérie Fonteyne, Nicolaas Lumen, Aurelie DeBruycker, Bieke Lambert et al. "Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial." (2017).
2. Phillips, Ryan, William Yue Shi, Matthew Deek, Noura Radwan, Su Jin Lim, Emmanuel S. Antonarakis, Steven P. Rowe et al. "Outcomes of observation vs stereotactic ablative radiation for oligometastatic prostate cancer: the ORIOLE phase 2 randomized clinical trial." JAMA oncology 6, no. 5 (2020): 650-659.
3. Mazzola, Rosario, Giulio Francolini, Luca Triggiani, Giuseppe Napoli, Francesco Cuccia, Luca Nicosia, Lorenzo Livi, Stefano Maria Magrini, Matteo Salgarello, and Filippo Alongi. "Metastasis-directed Therapy (SBRT) Guided by PET-CT 18F-CHOLINE Versus PET-CT 68Ga-PSMA in Castration-sensitive Oligorecurrent Prostate Cancer: A Comparative Analysis of Effectiveness." Clinical Genitourinary Cancer (2020).
4. Zelefsky, Michael J., Yoshiya Yamada, Carlo Greco, Eric Lis, Heiko Schöder, Stephanie Lobaugh, Zhigang Zhang et al. "Phase III Multi-Center, Prospective, Randomized Trial Comparing Single Dose 24 Gy Radiotherapy to a 3-Fraction SBRT Regimen in the Treatment of Oligometastatic Cancer." International Journal of Radiation Oncology* Biology* Physics (2021).


