
It is estimated that radical orchiectomy results in sperm impairment, but with the recovery of fertility after 2-3 years and a successful conception rate of 80%. For those undergoing retroperitoneal lymph node dissection (RPLND), the summarized data suggests that retrograde or anejaculation occurs in 0-14% of patients, with a successful subsequent conception rate of 59-78%. Among patients undergoing radiotherapy, 24% are azoospermic at 6 months, but with recovery at 24 months and a successful conception rate of 66%. As follows is a table displaying the relationship between radiation dose and the effect on fertility:

For patients undergoing chemotherapy, recovery of spermatogenesis occurs in 12 months if less than 2 doses of BEP are received, compared to 24 months for those receiving 2 or more doses; no recovery of spermatogenesis has been reported for patients receiving >5 cycles of BEP. Dr. Van Damme notes that it is important for patients receiving chemotherapy to avoid conception for 6-18 months.
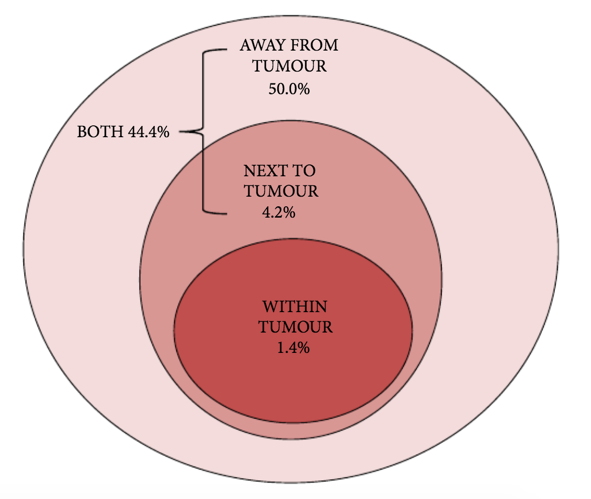
The EAU guidelines have a strong recommendation for discussing sperm banking with all men prior to starting treatment for testicular cancer, typically via cryopreservation of sperm. One interesting modality for sperm banking is onco-micro TESE. Moody and colleagues assessed the frequency of spermatogenesis in 103 patients with testicular cancer, finding that spermatogenesis was present in 70% (72/103) of patients, was widespread in 63% (45/72), and focal in 38% (27/72). Thus, these data would suggest that there may be support for a microsurgical approach to sperm retrieval at the time of orchiectomy to maximize success:
Dr. Van Damme states that management of post-treatment infertility in the post-chemotherapy setting should be TESE, while in the post-RPLND setting there is the opportunity to use alpha-adrenergics and/or electrostimulation. To conclude his presentation, Dr. Van Damme provided the following figure to summarize the testis cancer care pathway for the best oncological outcomes and maximal fertility preservation:

Presented by: Julien Van Damme, MD, PhD Student, CHU UCL-Godinne, CUSL-BXL, Pietrebais, Belgium
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md during the 18th Meeting of the EAU Section of Oncological Urology (ESOU21), January 29-31, 2021
References:
- Moody JA, Ahmed K, Yap T, et al. Fertility management in testicular cancer: the need to establish a standardized and evidence-based patient-centric pathway. BJU Int 2019 Jan;123(1):160-172.
- Moody JA, Ahmed K, Horsefield C, et al. Fertility preservation in testicular cancer – predictors of spermatogenesis. BJU Int. 2018 Aug;122(2):236-242.


