(UroToday.com) In a podium presentation in the ESU-ESOU-ERUS session at the 19th Meeting of the EAU Section of Oncological Urology, Dr. Nina Harke presented on considerations for choosing transperitoneal or retroperitoneal approaches for robotic partial nephrectomy. As is often done, she highlighted current guideline recommendations in this space. In Europe, the guidelines are non-comital with a recommendation that either an open, pure laparoscopic or robotic-assisted laparoscopic approach may be used “based on surgeon expertise and skills”. In contrast, the American Urological Association guidelines recommend that “a minimally invasive approach should be considered” when it would not compromise oncologic, functional, and perioperative outcomes. However, among patients opting for minimally invasive surgical approaches, neither guideline comments on considerations for transperitoneal or retroperitoneal surgery.
Dr. Harke emphasized that while it is important to decide and define our approach pre-operatively, we may need to be flexible and appropriate positioning on the flank with arms placed anteriorly may allow a transition from one approach to the other intra-operatively. She then discussed port placement. Clearly, this differs between transperitoneal and retroperitoneal approaches. While most are comfortable with port placement for transperitoneal partial nephrectomy, she highlighted important considerations for a retroperitoneal approach.
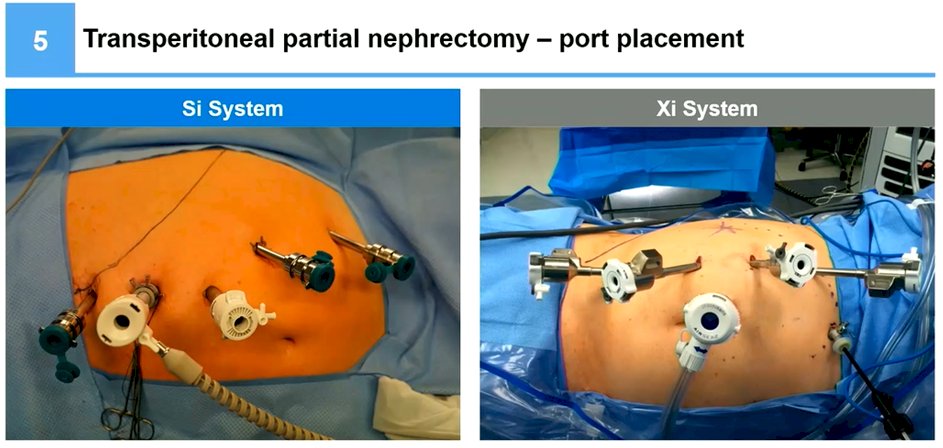
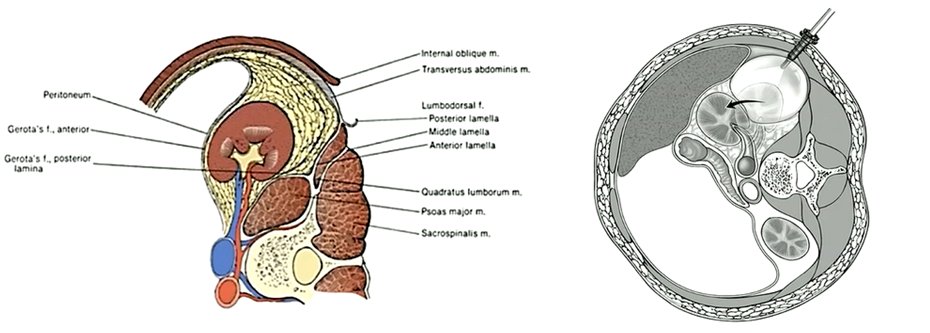
In the case of retroperitoneal surgery, she emphasized that, as with transperitoneal surgery, she prefers a relatively linear placement of the ports. She emphasized the importance of initially identifying the iliac crest and 12th rib as key anatomic landmarks. Then, using a combination of blunt dissection and palpation, the first port is placed in the axillary line. Following balloon dilation, two trocars are inserted directly onto her finger in order to avoid injury to adjacent structures. At this time, the peritoneum must then carefully be dissected off the abdominal wall to allow placement of the other ports without entering the peritoneum. Notably, she highlighted the value of using the needle to visualize the trajectory of ports prior to their placement. As with transperitoneal surgery, she highlighted that she prefers to use 4 robotic arms.

When beginning a program to approach retroperitoneal access, she emphasized that this is feasible using the da Vinci Si system, though this requires docking over the head.
She then highlighted data from six matched pair analyses comparing transperitoneal and retroperitoneal approaches. Five of six studies showed a shorter operative time with the retroperitoneal approach, approximately 20-30 minutes in most studies. This is explained primarily by a shorter time accessing the renal hilum. Using surgical videos to highlight, she demonstrated that the retroperitoneal approach allows direct access to the hilum when the fourth arm is used to hold up the kidney and the psoas muscle is followed to identify the hilar vessels.
As may be expected, tumor resection is equivalent between the approaches and as a result, warm ischemia time is comparable. She again utilized intra-operative footage to highlight this emphasizing that, particularly with the retroperitoneal approach, it is important to limit suction (especially when an AirSeal device is not being used) as this will diminish the operative space and increase bleeding.
She highlighted that there are particular scenarios in which a retroperitoneal approach may be preferred. In particular, transperitoneal surgery can be more difficult in patients with prior major open abdominal surgery. A comparative analysis showed that a retroperitoneal approach was much more commonly utilized in these patients and was able to achieve outcomes (including operative time, warm ischemia time, and major complication rates) that are comparable to those achieved in patients who did not have prior open abdominal surgery. However, she highlighted that extremes of body habitus (very thing and the obese) may make retroperitoneal surgery more difficult. However, retroperitoneal robotic-assisted partial nephrectomy is feasible in obese patients with comparable outcomes.
Dr. Harke highlighted that tumor location can contribute to decision making and that posterior tumors are more amenable to retroperitoneal approaches and these tumors have typically been the ones in which a retroperitoneal approach is used. However, this approach may be applied to anterior, lateral, and hilar tumors as well. Notably, tumor location (anterior, lateral, or posterior) does not appear to meaningfully affect operative time of ischemia time for patients undergoing retroperitoneal partial nephrectomy. However, other tumor characteristics may be important. She highlighted that she prefers a transperitoneal approach for cystic lesions given the small working space retroperitoneally and concerns of lesion rupture.
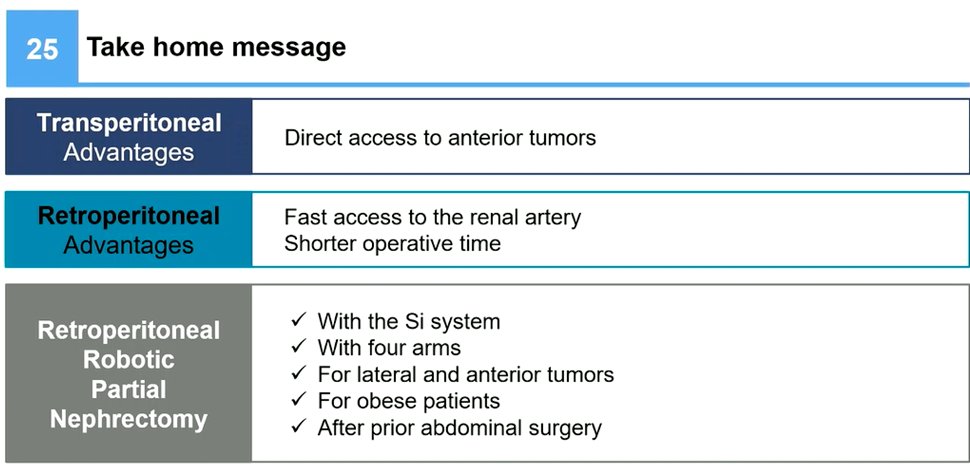
In conclusion, Dr. Harke highlighted that there are advantages to each approach but that retroperitoneal robotic partial nephrectomy is feasible in a variety of clinical scenarios.
Presented by: Nina Harke, Clinic for Urology, Hannover Medical School, Hannover, Niedersachsen, Deutschland


