(UroToday.com) In a podium presentation in the ESU-ESOU-ERUS session at the 19th Meeting of the EAU Section of Oncological Urology, Dr. Harke presented on complications following robotic assisted partial nephrectomy, along with their management. To begin, she highlighted the importance of a structured approach to assessing surgical complications. In 2004, Dindo published the classification of surgical complications comprising five grades, on the basis of the extent of intervention needed to manage them.
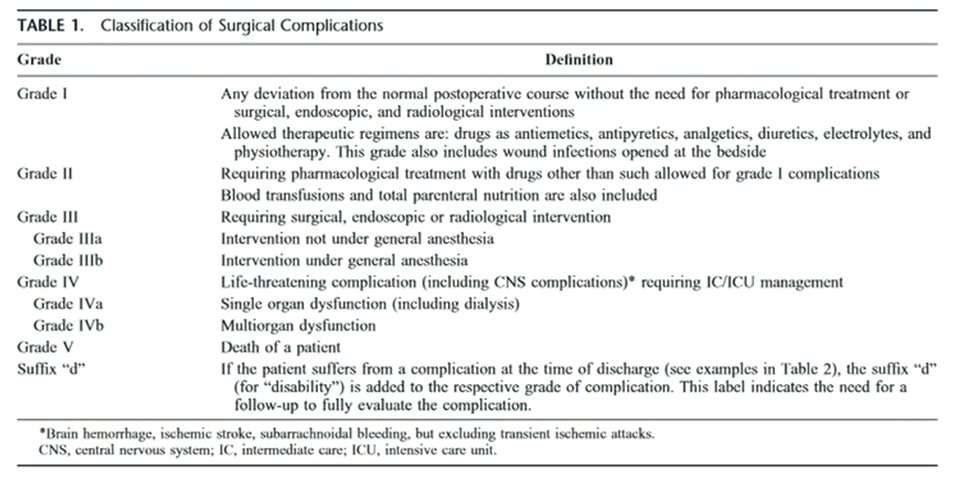
This approach has now become standard and, as of 2012, the EAU guideline panel recommended reporting of surgical complications using the Clavien-Dindo classification, with an appropriate rating of complication severity. Further, the panel emphasized the importance of providing a table of all complications including the corresponding grades. It is further important to understand who collected these data as well as relevant identifiable risk factors such as comorbidity scores, performance status, or American Society of Anesthesiologists (ASA) score. An assessment of complications should also consider readmissions and their causes and reoperations and their causes. Recently, an editorial in European Urology highlighted that approach has typically focused on short-term events following surgery (30, 60, and 90 days). However, a longer time horizon may be informative and necessary to comprehensively understand the morbidity of surgery.
In addition to these post-operative events, a systematic approach to the assessment of intra-operative complications is needed and a comparable grading system is available, again based on the severity of complication and degree of intervention required to manage it.
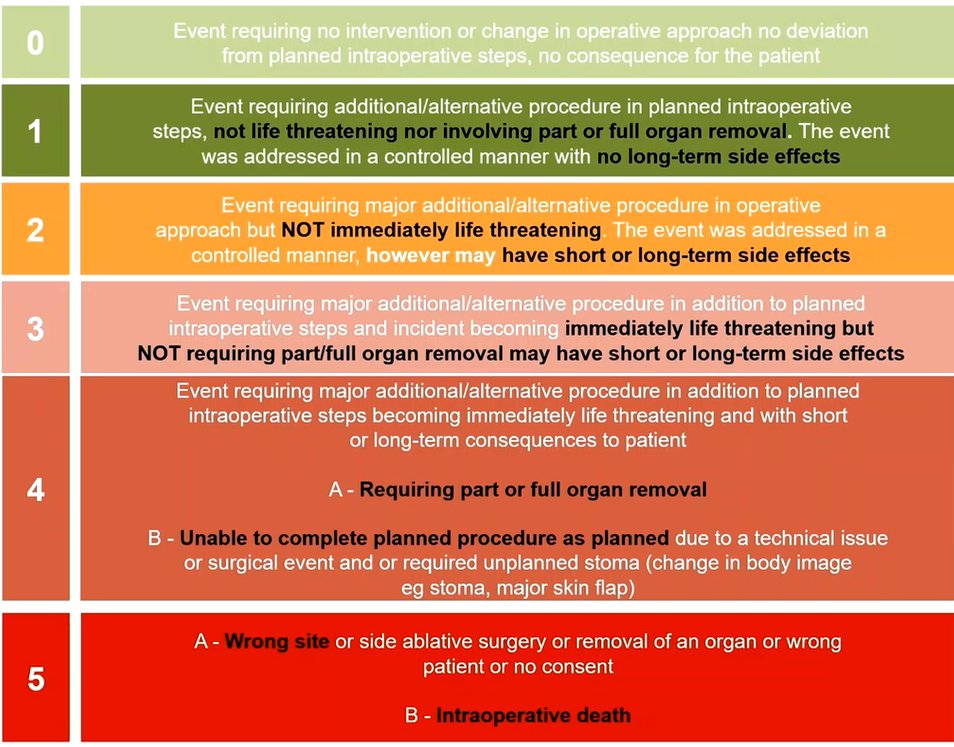
While a framework for these events is available, they are rarely reported. A review of nearly 30,000 partial nephrectomies performed in 2019 demonstrated than an intraoperative adverse event was reported in only 2.6% of cases.
Dr. Harke then moved to a discussion of specific intra-operative complications, with intra-operative video footage to guide the discussion. The first case was of an elderly lady on hemodialysis with a left side renal mass. During planned radical nephrectomy, intra-operatively, there was evidence of bleeding at the time of upper pole dissection. Further evaluation led to the identification of a superficial laceration to the pancreas which was managed with the placement of a hemostatic agent (or alternatively, suturing) and placement of a drain.
She highlighted that these pancreatic injuries are rare events (occurring in 0.2-2.6% of cases) with a preponderance for left sided nephrectomies. They are rarely identified intraoperatively and often are treated conservatively with drain placement.
The second case presented was of a lower pole cystic lesion. Taking a retroperitoneal approach, the operating surgeon identified a difficult dissection requiring cautery and sharp dissection. As a result of the inability to blunting dissect tumor planes, there was a parenchymal injury leading to bleeding. After this was mitigated, there was inadvertent clamping of only the segmental artery which led to significant bleeding during the course of tumor excision. While Dr. Harke recommended the use of a lap pad and selective suturing the manage this, the operating surgeon increased the pace of tumor excision, leading to inadvertent tumor rupture of the cystic lesion.
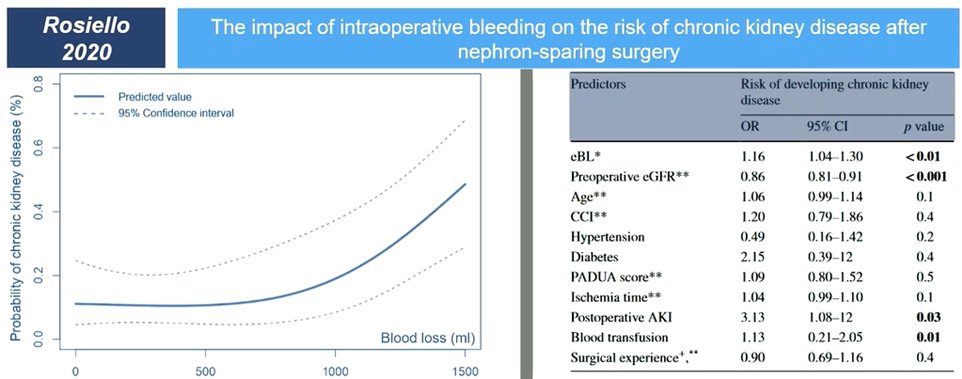
In this context, Dr. Harke noted that adhesive fat is associated with an increased operative time and increased transfusion rate but not increased complication rates. However, intraoperative hemorrhage, as measured with the estimated blood loss, is associated with long-term risk of chronic kidney disease.
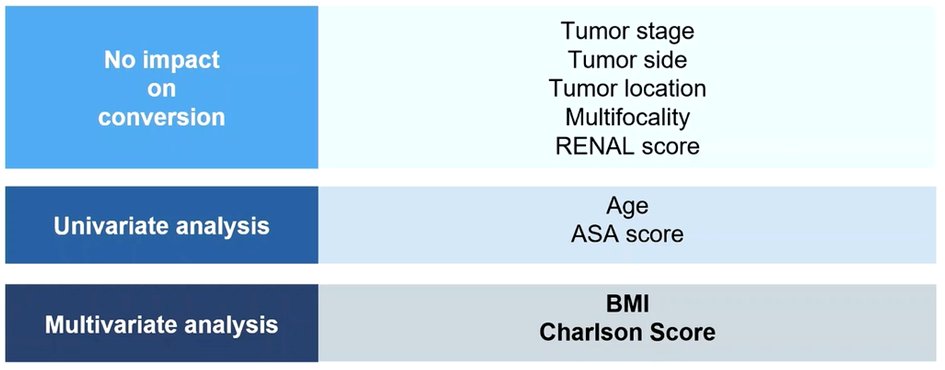
She noted that, sometimes, complications may prompt the need for conversion. This is an uncommon event in patients undergoing partial nephrectomy and occurs more commonly in older patients, with higher BMI, higher Charlson comorbidity, and higher ASA score. Interestingly, tumor complexity (measured with RENAL scores, and comprising tumor stage, location, multifocality, and side) did not meaningfully differ. Most patients had a conversion to a robotic radical nephrectomy (24/25 in a cohort of 501 patients overall).
In managing tumor spillage, she emphasized the importance of using suction and irrigation to ensure that disease is not left behind. Notably, rupture of cystic renal masses is relatively common: even in experienced centers, intra-operative cyst rupture is seen in nearly 19% of cases. This occurs similarly whether open or robotic surgery is performed and BMI, tumor size, surgeon experience, anticoagulation, and malignant histology do not appear to be predictive. Fortunately, tumor rupture does not appear to be associated with worse long-term oncologic outcomes.
Next, Dr. Harke discussed urine leaks following partial nephrectomy. A recent review demonstrated that this is less common following robotic partial nephrectomy (0.5-4%), compared to laparoscopic partial nephrectomy (1-16%) or open partial nephrectomy (1-17%). Most of these patients have a delayed presentation (13 days following surgery) and can be managed with drainage of the urinoma, unobstructed distal urinary flow, and prevention of infection. She emphasized that this may be prevented with intra-operative identification of entry into the collecting system and direct suture repair.
Presented by: Nina Harke, PD Dr. med., Head of Robotic Urology, Assistant Professor Hannover Medical School, Hannover Medical School, Hannover, Germany

