Among clinical N0 patients, approximately 20% will still harbor occult metastases, and currently, there are no useful/validated nomograms available for penile cancer and predicting which clinical N0 patients are clinical N positive. For these clinical N0 patients, non-invasive inguinal staging techniques remain inaccurate. Inguinal ultrasound has a low sensitivity (39%), but with the addition of fine needle aspiration does have a relatively high specificity. A positive fine needle aspiration would then allow patients/clinicians to proceed to inguinal lymph node dissection confidently and thus reduce the number of groins undergoing aggressive staging. Furthermore, CT or MRI cannot detect micrometastases reliably (sensitivity approximately 20-40%), and neither can PET/CT with sensitivities of ~57% and specificities of 88-92% in clinical N0 patients. Therefore, at the present time, surgical staging remains indispensable for clinical N0 patients.
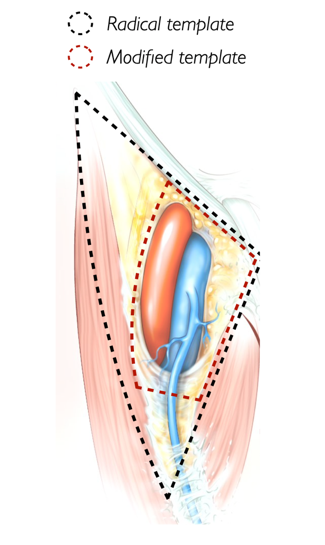
Invasive staging options have historically included radical inguinal lymph node dissection, which has the highest sensitivity, but also has the highest morbidity (50-65% complication rate), and results in over-treatment of 80% of men with clinical N0 disease. Over the last decade or so, clinicians have moved toward the modified inguinal lymph node dissection, which has good sensitivity, but still with a potential morbidity rate of 38-58%. The templates of these dissections are as follows:
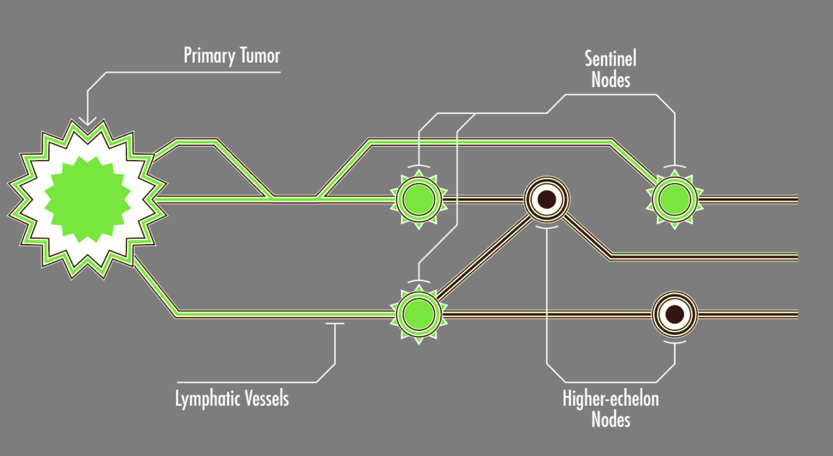
The dynamic sentinel node biopsy is an option for maintaining a good sensitivity for detecting lymph node metastases, but with a much lower complication rate (6-21%) compared to inguinal lymph node dissection. The sentinel lymph node concept is such that the sentinel node is the first site of nodal metastasis, where a pN0 at the sentinel node is equivalent to a pN0 in the ipsilateral lymph node basin, thus the sentinel node biopsy spares patients an unnecessary lymph node dissection:
The evolution of the sentinel node procedure dates back to the 1990s, first pioneered in melanoma and breast cancer, finally gaining momentum in penile cancer in the early 2000s.1 The traditional sentinel node procedure for penile cancer is as follows:
- Preoperative lymphoscintigraphy after injection of 99mTc-nanocolloid
- Intraoperative gamma probe and blue dye
- The false-negative rate for this technique has been 5-15%, but better at high volume centers
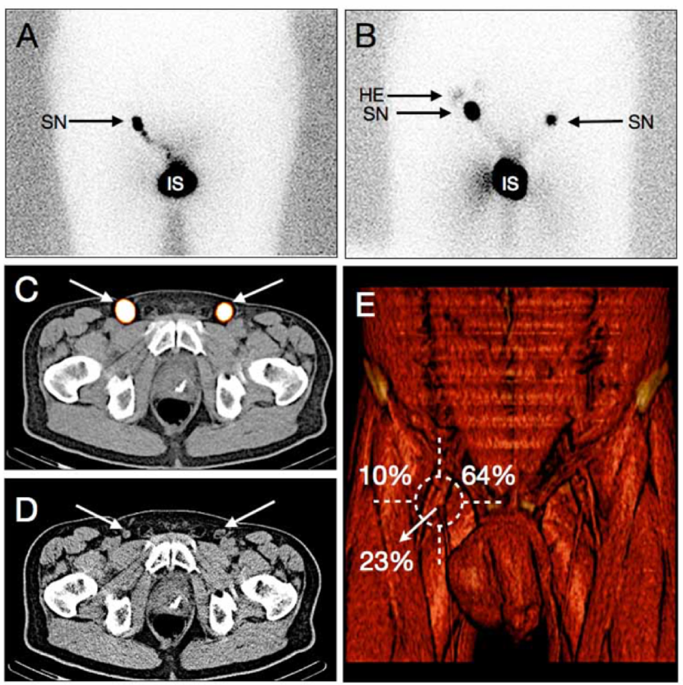
Innovations to improve dynamic sentinel node biopsy include the utilization of SPECT/CT. Using SPECT-CT (i) increases sensitivity (detection of more sentinel nodes), (ii) allows for three-dimensional reconstruction (differentiation between sentinel nodes and higher echelon pelvic nodes), (iii) helps visualize the sentinel node in cases where non-visualization can be 10-35%, and (iv) CT imaging can identify pathologic nodes that did not pick up the tracer:
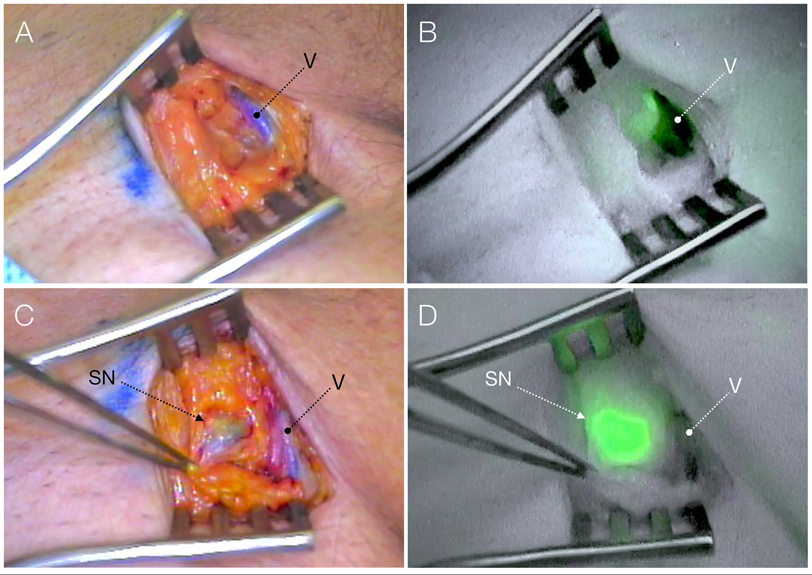
Additional innovations include dual labeled/hybrid tracers, which combines traditional radioactive 99mTc-nanocolloid and fluorescent indocyanine green, allowing radio- and fluorescent guidance with ICG-99mTc-nanocolloid – the best of both worlds. In a recently published study in European Urology from Dr. Brouwer’s group, they aimed to confirm the reliability of ICG-99mTc-nanocolloid and to assess whether blue dye is still of added value.2
This study included 400 men with ≥T1G2N0 penile cancer that were staged with sentinel biopsy; sentinel nodes were preoperatively identified with lymphoscintigraphy and SPECT-CT. Intraoperatively, sentinel nodes were detected via gamma tracing, blue staining, and fluorescence imaging. Among 740 groins assessed, all preoperatively defined sentinel lymph nodes (n=1,163) were localized intraoperatively. Among all excised sentinel lymph nodes, 98% were detectable with gamma probe and 96% were visible with fluorescence imaging. In patients who received ICG-99mTc-nanocolloid and blue dye, fluorescence imaging yielded a 39% higher sentinel node detection rate than blue dye (95% CI 36-43%, p<0.001). Furthermore, of the sentinel nodes that were tumor positive, 100% were intraoperatively visualized by fluorescence imaging, whereas only 84% of the positive nodes stained blue.
Both the National Comprehensive Cancer Network (NCCN) and European guidelines support dynamic sentinel node biopsy. The European Association of Urology (EAU) provides a strength rating of ‘strong’ for patients with clinical N0 nodes and ≥T1G2 primary tumor to undergo either bilateral modified inguinal lymphadenectomy or dynamic sentinel node biopsy, which is echoed by the NCCN guidelines for the same patient population.
Dr. Brouwer concluded his presentation of minimally invasive evaluation techniques for staging the inguinal nodes with the following take-home messages:
- Clinical node status: should initially be assessed by palpation and ultrasound plus fine needle aspiration
- Clinical node-positive patients should have a fine needle aspiration, followed by either a CT or PET/CT scan to complete distant staging
- For clinical N0 patients, approximately 20% still harbor occult metastases
- Since imaging options lack sensitivity, invasive staging remains necessary in intermediate and high-risk clinical N0 patients
- For appropriate staging, there is a balancing act between optimizing diagnostic accuracy while minimizing morbidity
- Currently, Dr. Brouwer advocates for dynamic sentinel node biopsy, although he notes there is a learning curve to the procedure
Presented by: Oscar Brouwer, MD, PhD, FEBU, The Netherlands Cancer Institute, Antoni van Leeuwenhoek Hospital, Amsterdam, The Netherlands
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia Twitter: @zklaassen_md during the 1st Global Society of Rare Genitourinary Tumors Virtual Summit, December 11-12, 2020
References:
- Horenblas S, Jansen L, Meinhardt W, et al. Detection of occult metastasis in squamous cell carcinoma of the penis using a dynamic sentinel node procedure. J Urol 2000 Jan;163(1):100-104.
- Dell’Oglio P, de Vries HM, Mazzone E, et al. Hybrid Indocyanine Green-99mTc-nanocolloid for single-photon emission computed tomography and combined radio- and fluorescence-guided sentinel node biopsy in penile cancer: Results of 740 inguinal basins assessed at a single institution. Eur Urol 2020 Dec;78(6)865-872.


