(Urotoday.com) The newly formed Global Society of Rare Genitourinary Tumors (GSRGT) held its inaugural meeting December 11-12, 2020 focusing on penile and testicular cancer. The session held Saturday, December 12th focused on testis cancer. In this session, Dr. Andrea Necchi presented on the management of early-stage (CSII) non-seminoma (NSGCT).
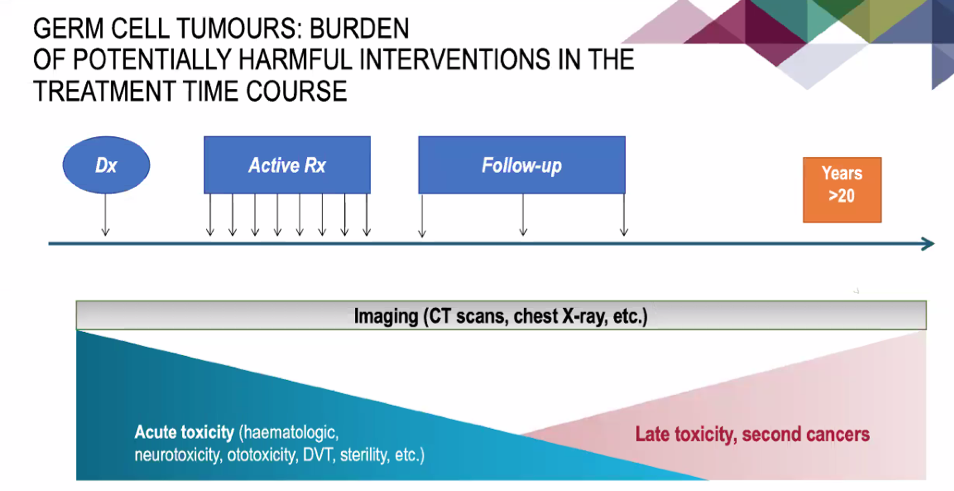
To begin, he emphasized the importance of balancing the efficacy of therapy and the long-term toxicity of treatment for patients with CSII NSGCT.
In this context, he identified that distinguishing between CSI and CSII disease is of importance. Notably, not all small volume changes on CT scan represent disease. Further, 10-40% of patients who are clinically CSII are found to have uninvolved lymph nodes (pathologic CSI).
In this context, Dr. Necchi opened the question to the panel about how to manage a patient with this type of questionable lymph node involvement. 
Dr. Robert J. Hamilton, MD, MPH, FRCSC, Department of Surgical Oncology Urology and Assistant Professor, at the University of Toronto was the first to respond, indicating that there is no need to rush into intervention and, instead, suggesting relatively short interval imaging. Further, he emphasized that a period of delay may help clarify the burden of disease to guide treatment choices between retroperitoneal lymph node dissection (RPLND) and chemotherapy.
Dr. Siamak Daneshmand, MD, Associate Professor of Urology, Director of Clinical Research at the Keck School of Medicine, at USC Univerity of Southern California, agreed that this was not convincing evidence of nodal involvement and that he would recommend re-imaging in 6 to 8 weeks.
Dr. Silke Gillessen, Professor, Medical Oncologist, and Director of the IOSI (Oncology Institute of Southern Switzerland), emphasized that this approach is suitable in the context of serum marker negative disease. Further, she highlighted that inflammatory changes on CT scan can be reduced by performing CT scans prior to orchiectomy.
Dr. Craig Nichols, MD FASCO, SWOG Executive Officer, Founder/Director Testicular Cancer Commons, suggested that almost all patients with CS IIA should have repeat imaging/markers in 6-8 weeks to clarify diagnosis prior to definitive intervention. Further, this clinical context provides a good role for miR-371.
Dr. Darren R. Feldman, MD, Medical Oncologist, Chair, Quality Assurance, Department of Medicine at Memorial Sloan Kettering Cancer Center postulated that how you approach stage I changes how you approach this case of equivocal stage IIa disease: if patients are being considered for RPLND in the context of CSI disease, then these equivocal findings should not inherently change treatment decisions.
Dr. Alejandro Rodriguez highlighted that in some regions of the world, follow-up may be more difficult and may suggest a preference for intervention.
In this context, Dr. Phillip Spiess, genitourinary oncologist and the assistant chief of surgical services at the Moffitt Cancer Center raised the question of patient compliance and insurance but Dr. Daneshmand emphasized that this should not be the primary driver of decisions as physicians are often unable to accurately predict compliance.
Dr. Necchi then presented a number of considerations in the treatment approach to patients with CSIIA/B disease, emphasizing the cancer cure is high regardless of approach and thus minimizing toxicity should be a key consideration in treatment choice.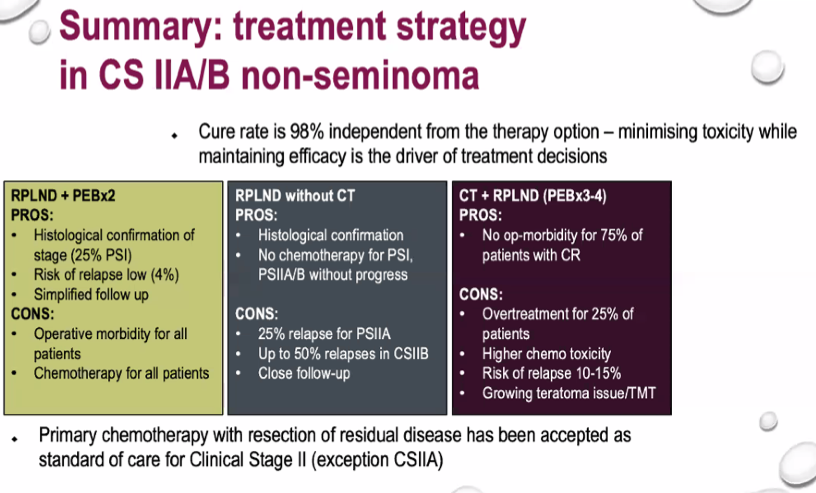
Dr. Daneshmand suggested that in patients with CSIIA disease, he strongly advocated surgery as it is curative in up to 80% and may avoid much of the long-term toxicity associated with chemotherapy. Among patients with CSIIB disease, he emphasized the heterogeneity based on the burden of disease and that distinction between CSIIA and CSIIB are not based on biological differences.
Dr. Stephenson, MD FRCSC FACS, Director, Urologic Oncology, Professor of Surgery, Rush University Medical Center highlighted the importance of this qualitative assessment of imaging as findings indicative of potential teratoma would favor resection. Finally, Dr. Hamilton emphasized that patients with de novo CSIIA/B differ from patients with comparable burdens of disease follow relapse after surveillance for clinical stage I (CSI) in that surveillance patients have had a period of observation to allow assessment of the natural history of the disease, excluding other systemic spread.
Presented by: Andrea Necchi, MD, Associate Professor, Vita-Salute San Raffaele University, Head of Genitourinary Medical Oncology, IRCCS San Raffaele Hospital and Scientific Institute, Milan, Italy
Written by: Christopher J.D. Wallis, MD, Ph.D., Instructor in Urology, Vanderbilt University Medical Center, Nashville, Tennessee @WallisCJD on Twitter during the 1st Global Society of Rare Genitourinary Tumors Virtual Summit, December 11-12, 2020


