(Urotoday.com) The newly formed Global Society of Rare Genitourinary Tumors (GSRGT) held its inaugural meeting, focusing on penile and testicular cancer. The session held Saturday, December 12th focused on testis cancer. In this session, Dr. Andrew Stephenson presented on the management of early-stage clinical stage I (CSI) seminoma.
Dr. Stephenson began by emphasizing that 70-80% of patients with CSI non-seminoma are cured by orchiectomy alone. Thus, considering treatment options of surveillance, retroperitoneal lymph node dissection (RPLND), and adjuvant bleomycin-etoposide-cisplatin (BEP) chemotherapy x 1 cycle, we need to consider compliance and patient preference, the risk of occult systemic disease, and the morbidity of treatment.
In the context of RPLND, Dr. Stephenson highlighted that older data may not apply to clinical practice as trends in patient selection (for example from 1989-1998 vs 1999-2002) suggest that improved outcomes among patients treated more recently.
As the lead author in the American Urologic Association (AUA)/American Society of Clinical Oncology (ASCO) guidelines in this space, he emphasized their recommendations: for patients with CSIA disease, the guidelines recommend surveillance as the preferred approach with RPLND and BEP chemotherapy as appropriate alternatives while in CSIB, all three options can be recommended.
In terms of surveillance, he discussed the importance of risk-adapted surveillance. In particular, he noted that the risk of occult metastasis in CSI non-seminoma is approximately 40-50% in patients with lymphovascular invasion while less than 15% among those without LVI.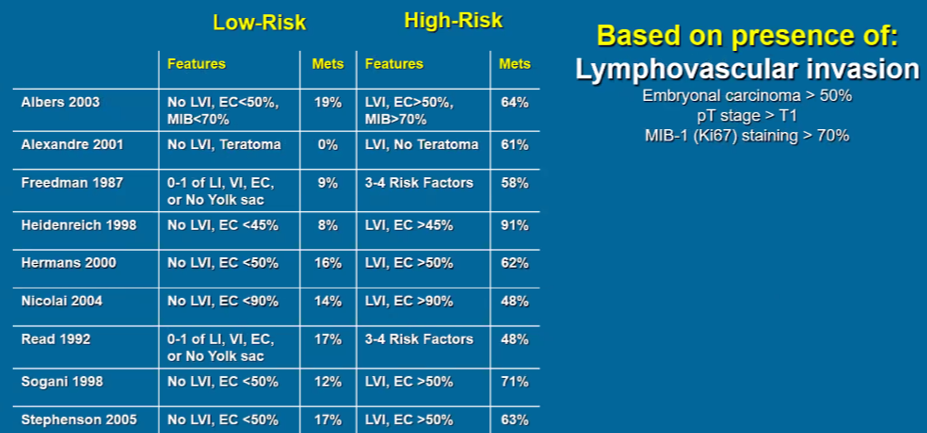
When considering patients for surveillance, he highlighted the importance of critically reviewing CT scans given the difference between a truly “pristine” scan and one with small, sub-centimeter lymph nodes. In particular, he emphasized that any lymph node >5mm in the primary landing zone should be considered suspicious for metastasis.
Considering treatment options for these patients, he further highlighted the potential role of miR-371 as a novel biomarker. In this disease space, it may be useful to detect occult disease beyond the testicle.
In terms of selecting treatment approaches, Dr. Stephenson highlighted some of his own work in decision analysis modelling showing that the preferred treatment approach differs according to the patient’s risk of relapse.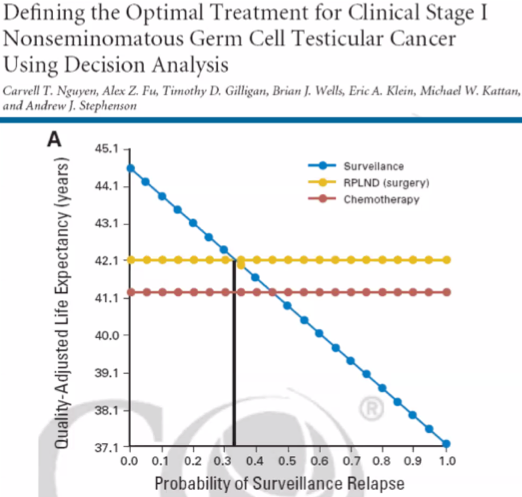
Nguygen et al. J Clin Oncol 2010
Dr. Stephenson highlighted randomized data comparing BEP x1 to RPLND which concluded that the chemotherapy approach was superior. However, he highlighted limitations to these data, in particular, that RPLND was performed at many institutions, a large number of which were low volume, and as a result, 9 of 15 relapses among surgically treated patients were local suggesting inadequate surgical approach.
Additionally, Dr. Stephenson emphasized that while teratoma is a “benign” entity, there is uncertain biology with the potential for growing teratoma syndrome, malignant transformation, and late recurrence. Further, the absence of teratoma in the testis does not preclude teratoma in the retroperitoneum. Given teratoma’s resistance to chemotherapy, surgical resection is required.
For patients undergoing RPLND, Dr. Stephenson highlighted that the AUA guidelines recommend that accepted anatomic principles should be adhered to, regardless of whether an open or minimally-invasive approach is used. Further, a full, bilateral template was endorsed in all with suspicious lymph nodes on imaging or intra-operative assessment and in those with somatic-type tumors in the primary.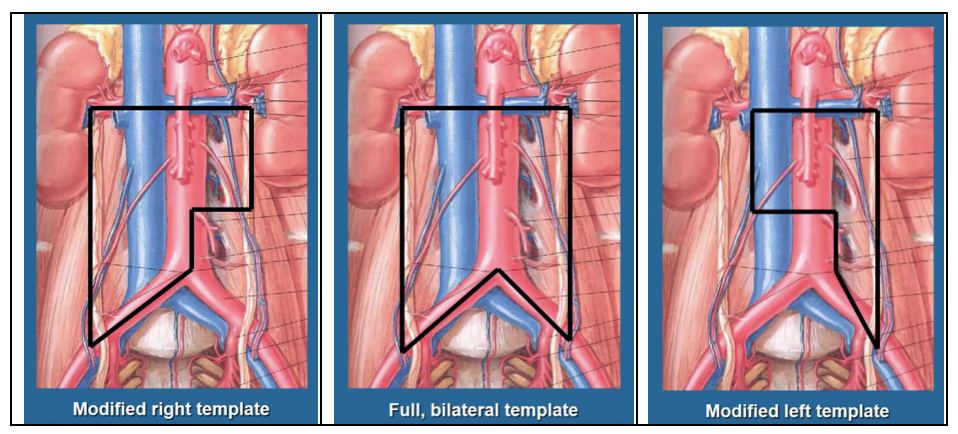
In closing, he emphasized that long-term survival in CSI non-seminomatous germ cell tumors (NSGCT) approaches 100%. Thus, strong consideration should be undertaken for surveillance among those at low risk of relapse. In those opting for treatment, BEP x1 and RPLND may be considered. Moving forward, use of miR-371 may change this paradigm. He closed with a quote from Dr. Swanson, emphasizing the risk from treatment-related toxicity.
Presented by: Andrew J. Stephenson, MD FRCSC FACS, Director, Urologic Oncology, Professor of Surgery, Rush University Medical Center
Written by: Christopher J.D. Wallis, MD, Ph.D., Instructor in Urology, Vanderbilt University Medical Center, Nashville, Tennessee @WallisCJD on Twitter during the 1st Global Society of Rare Genitourinary Tumors Virtual Summit, December 11-12, 2020


