He began by emphasizing that testicular cancers represent a paragon of successful multimodal treatment with extremely high cure rates and long-term survival. Thus, there is a large need to prioritize survivorship and consider approaches to reduce the long-term burden of treatment.
PRIORITIZING SURVIVORSHIP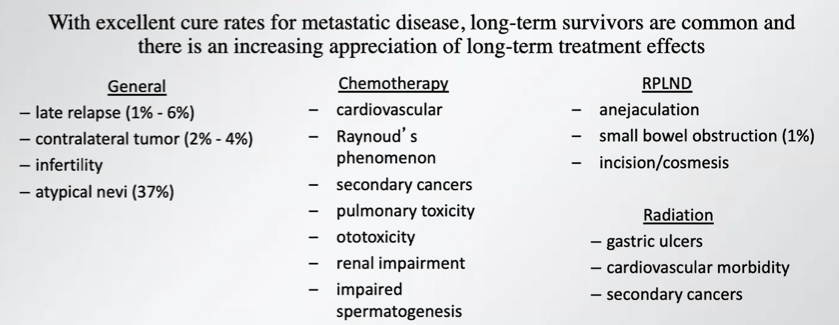
Dr. Eggener highlighted that approximately 30% of patients with germ cell tumors received non-guideline directed care. Much of this relates to inappropriate imaging (44%) and overtreatment (40%) while a minority of patients have undertreatment (16%). Non-guideline directed care was associated with higher rates of relapse-free survival (hazard ratio 2.49, 95% confidence interval 1.61-3.85) as well as worse quality of life and more financial difficulties.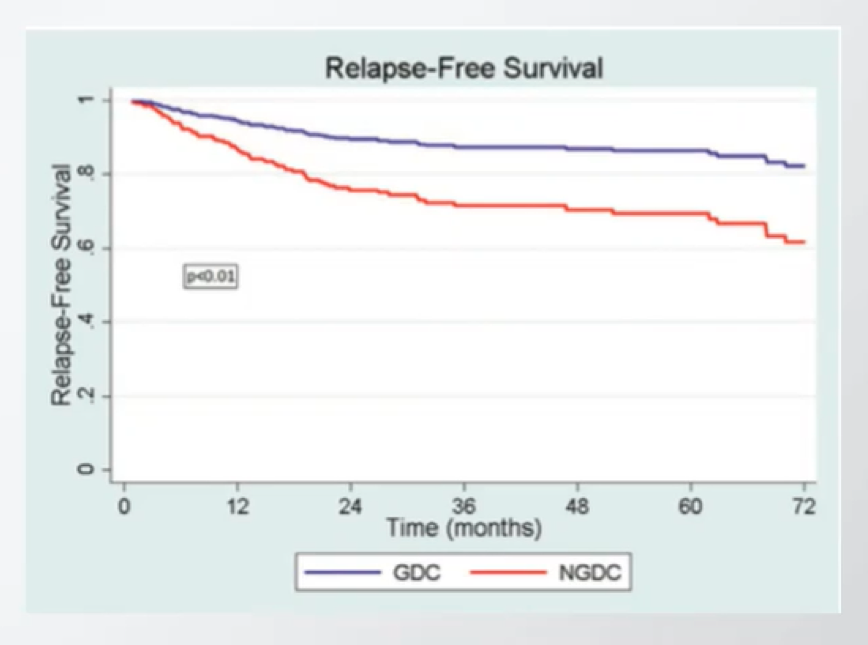
Dr. Eggener highlighted that, based on data from the National Cancer Database, more than half of United States hospitals perform 2 or fewer retroperitoneal lymph node dissection (RPLND)s annually. However, it is known that treatment at a high-volume hospital is an independent predictor of improved survival. Thus, AUA and NCCN guidelines recommend consideration of consultation or referral at a high-volume center.
In the context of patients with low-volume retroperitoneal lymph node disease, Dr. Eggener highlighted recommendations from the 2019 AUA guidelines recommending that solitary lymph nodes less than 15mm should be approached cautiously, particularly where they are outside the primary landing zone. Rather than initial resection, consideration of repeat imaging and markers in 4-8 weeks should be undertaken. This is because up to 40% of patients with clinical stage IIA disease are pN0 following RPLND. 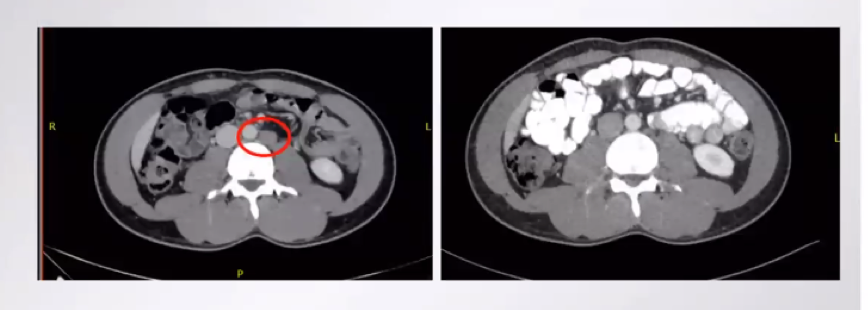
Dr. Eggener then highlighted heterogeneity within CS IIB. Based on the formal definition, he highlighted that the largest node should be 2-5cm and there should be no more than 5 enlarged nodes. Highlighting the heterogeneity of this disease category, he suggested a subset of IIb with a solitary node <3cm in the landing zone for whom local therapy should be favored, in contrast to a subset of IIB with nodes greater than 3cm, multiple nodes, or those in unexpected locations for whom systemic approaches may be prioritized.
He then emphasized the high rates of cure (95% in patients with good risk, 80% in intermediate-risk, and 50% in poor risk) in stating the importance of urologists to understand and master this disease, across all of its elements and permutations.
In this context, he then highlighted the role of post-chemotherapy RPLND for patients with non-seminoma who have residual masses >1cm following primary chemotherapy.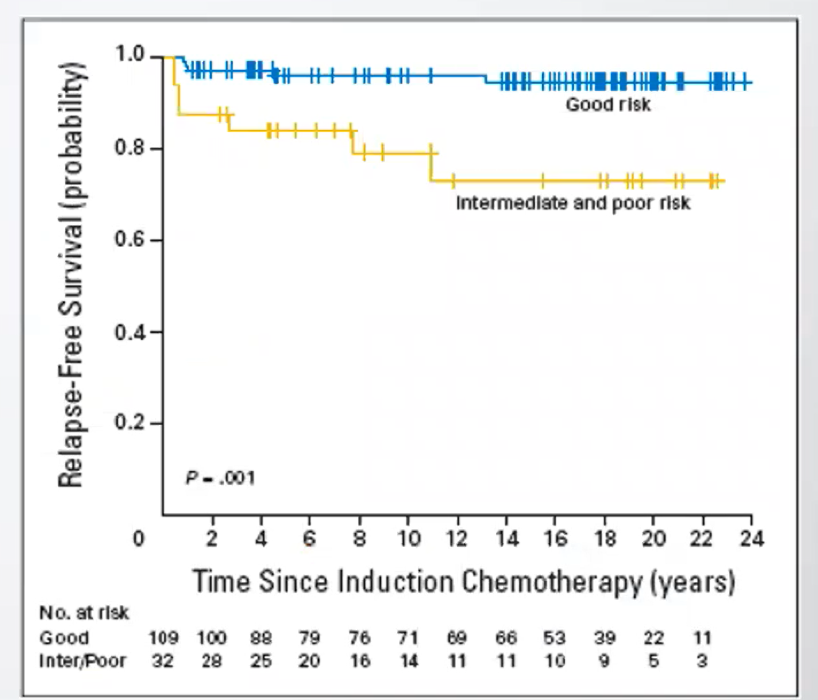
However, for patients with residual masses <1cm, he highlighted the decision node between surveillance and RPLDN. He emphasized data from Indiana demonstrating that, with a surveillance approach for patients with residual masses <1cm, relapse free survival was particularly good for patients with good-risk disease (95% at 15-years) compared to those with intermediate or poor risk (73% at 15-years).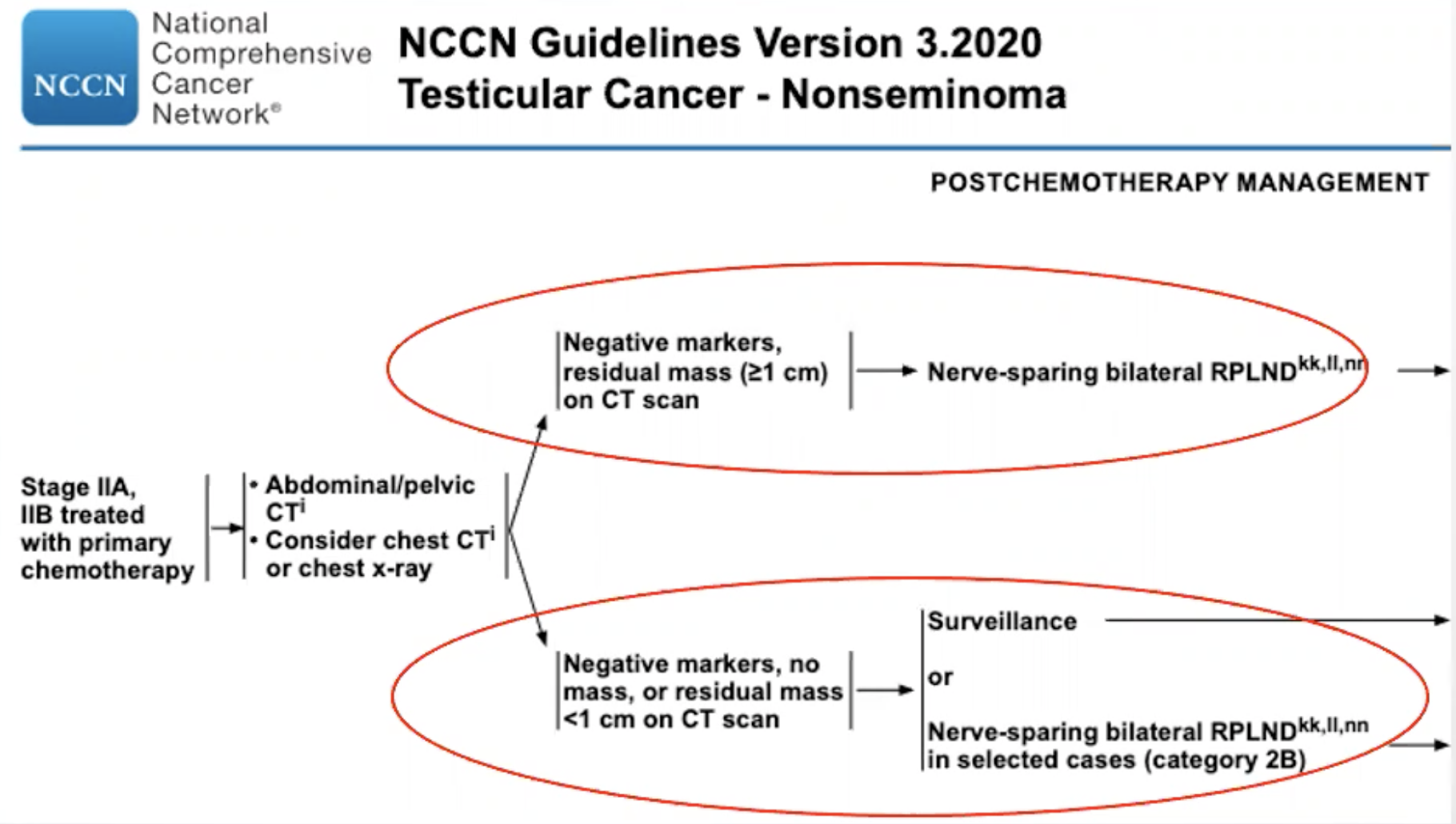
For patients who do undergo post-chemotherapy RPLND, the presence of viable germ cell tumor is typically considered an indication for two cycles of adjuvant EP following complete resection. However, in the context of de-escalating care, he highlighted data from Dr. Fizazi and others showing that observation may be reasonable for patients with the International Germ Cell Cancer Collaborative Group (IGCCCG) good-risk disease who have <10% viable tumor and complete resection. These nuances highlight that knowing the disease and the data is critical for de-escalation treatment approaches. For example, in the context of a post-chemotherapy seminoma mass, he emphasized that he looks for reasons not to perform an RPLND. Thus, he now advocates only performing RPLND for patients with SUV >5 on PET-CT, a growing mass, or a biopsy proving active cancer.
Considering the future, he discussed the role of minimally-invasive surgical approaches. Clearly, in the context of de-escalating the morbidity of treatment, minimally-invasive surgery is an obvious way to reduce the burden of treatment if proven to be oncologically equivalent. Further, use of novel biomarkers, including miR-371 may have dramatic influence across the spectrum of germ cell tumors, including the potential to target therapy for patients with active disease.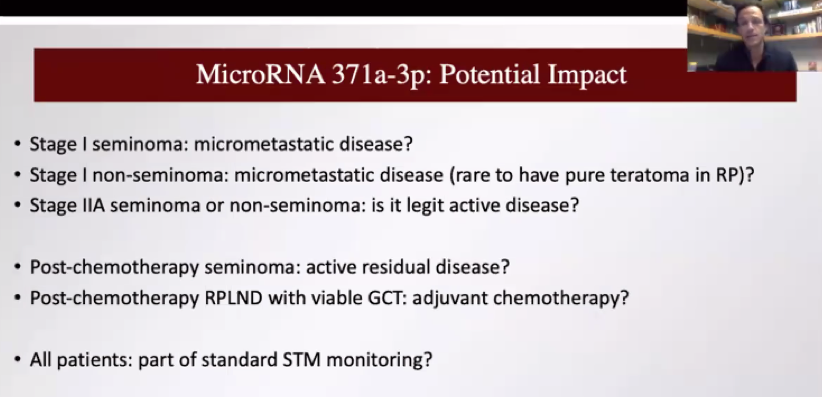
Dr. Eggener concluded that we should evolve to more targeted approaches, identifying ways to de-escalate care to compromise the quality of life or cure.
Presented by: Scott Eggener, MD, Professor of Surgery, (Urologic Oncology) and Radiology, The University of Chicago
Written by: Christopher J.D. Wallis, MD, Ph.D., Instructor in Urology, Vanderbilt University Medical Center, Nashville, Tennessee @WallisCJD on Twitter during the 1st Global Society of Rare Genitourinary Tumors Virtual Summit, December 11-12, 2020


