(UroToday.com) The 2024 IBCN annual meeting included a bladder cancer session, featuring a presentation by Dr. Vignesh Packiam discussing the validation of an artificial intelligence-powered pathology assay and comparison to the EAU 2021 guidelines on the prediction of muscle-invasive progression post BCG in an international 12-center cohort.
High-risk non muscle invasive bladder cancer (NMIBC) is associated with a 5-year recurrence-free survival rate as low as 25% despite the use of intravesical therapy with 30-50% of patients developing BCG unresponsive disease. Although intravesical BCG is the first-line therapy for NMIBC, there is a lack of biomarkers to identify those who will progress to muscle-invasive disease. These investigators used previously developed deep learning-based histologic assays that extract interpretable features from BCG-naïve TURBT digitized pathology slides to predict muscle invasive progression following BCG and compared with the EAU guidelines risk stratification.
Pre-intravesical BCG TURBT-derived digital whole slide images and clinical data were obtained for BCG-naïve AUA high-risk NMIBC cases diagnosed between 2007-2022 and treated with adequate BCG therapy from 12 academic centers. Whole slide images were analyzed through a segmentation and geometric feature extraction pipeline. This was then input for a multivariable Cox proportional hazards model to identify features correlated with recurrence-free survival: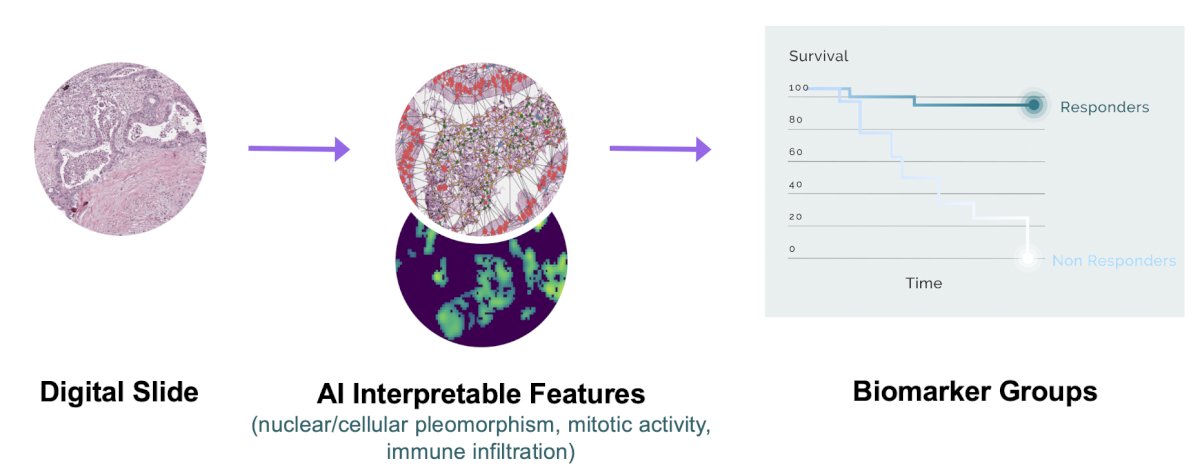
Cases were classified into high risk (upper 10%) and low risk (bottom 90%) of progression (PFS-high vs low) and risk of BCG unresponsive disease. Comparisons were made with EAU (progression) risk groups.
There were 944 high-risk NMIBC cases (development cohort: 303; validation cohort: 641) with a median follow-up of 36 months included (HGTa: 34.1%; HGT1: 54.8%; any CIS: 31.4%). In the validation set, patients in the PFS-high had significantly inferior PFS (HR 3.9, 95% CI 2.8-5.4 p<0.001) versus the PFS-low group: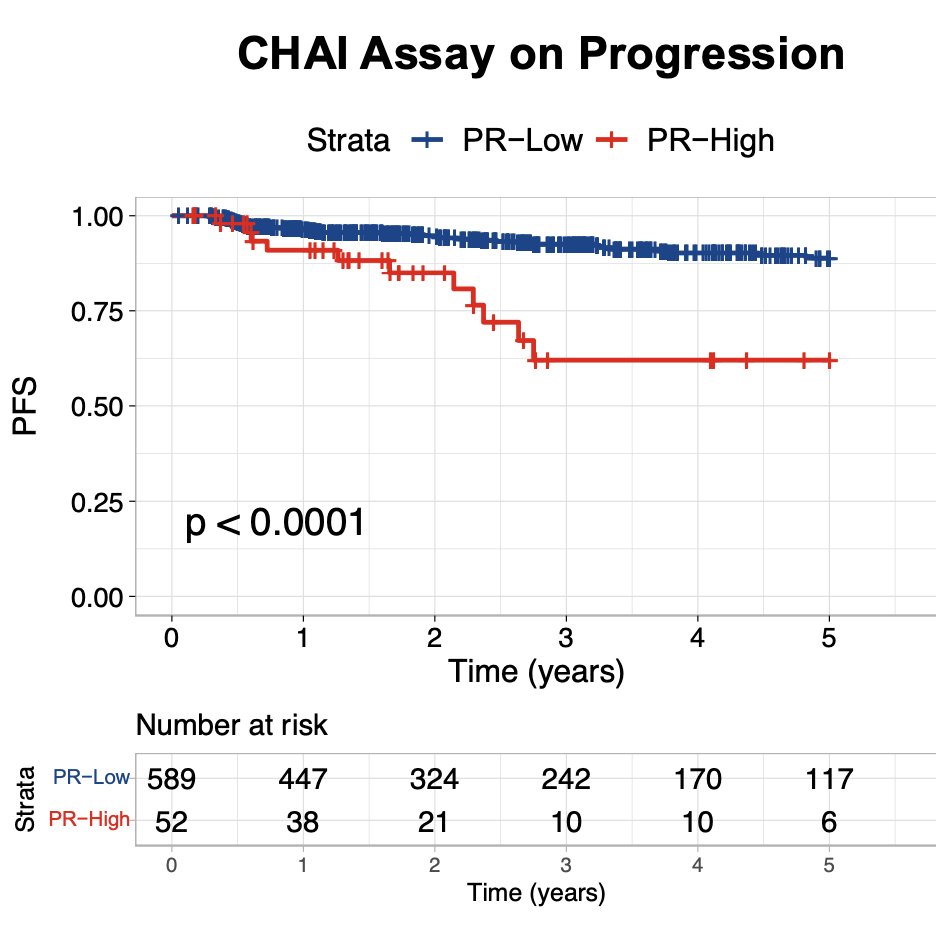
Artificial intelligence biomarkers performed independently of clinicopathologic risk factors for NMIBC and were superior to the EAU 2021 risk calculator in determining progression risk (vs EAU “very high risk” versus “high risk”: HR 1.51, p = 0.029):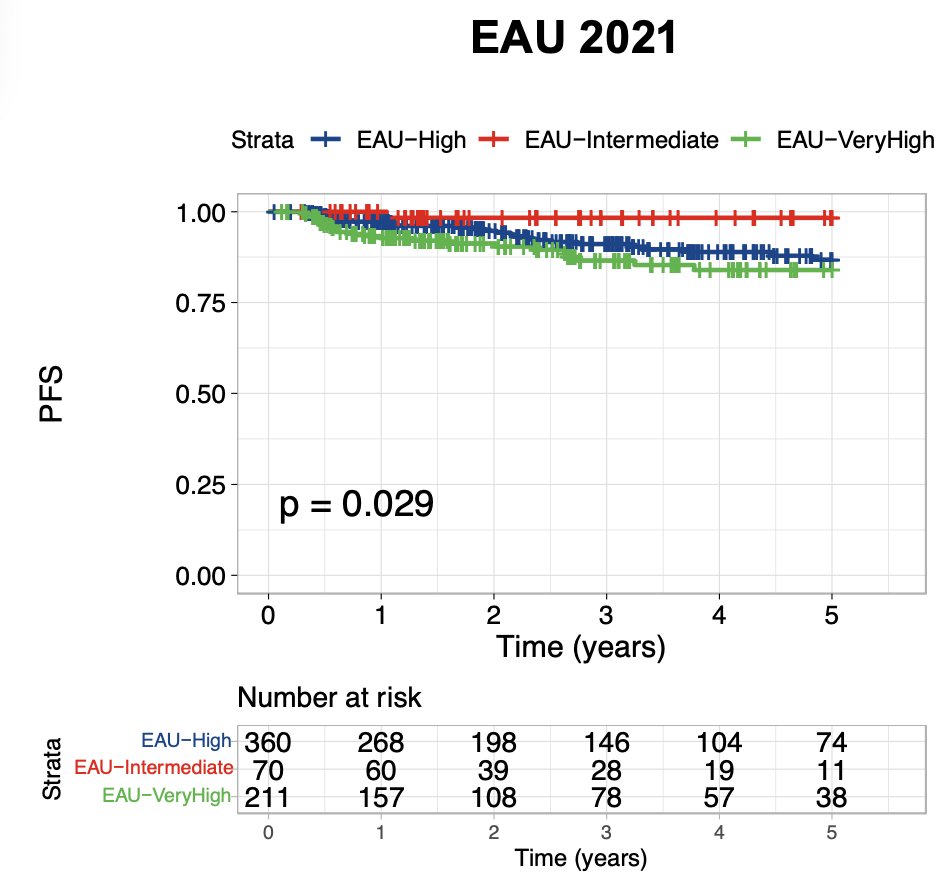
The BCG unresponsive disease positive group also had shorter time to BCG unresponsive disease (HR 2.3, 95% CI 1.9-2.8 p<0.0001) versus the BCG unresponsive disease negative biomarker group: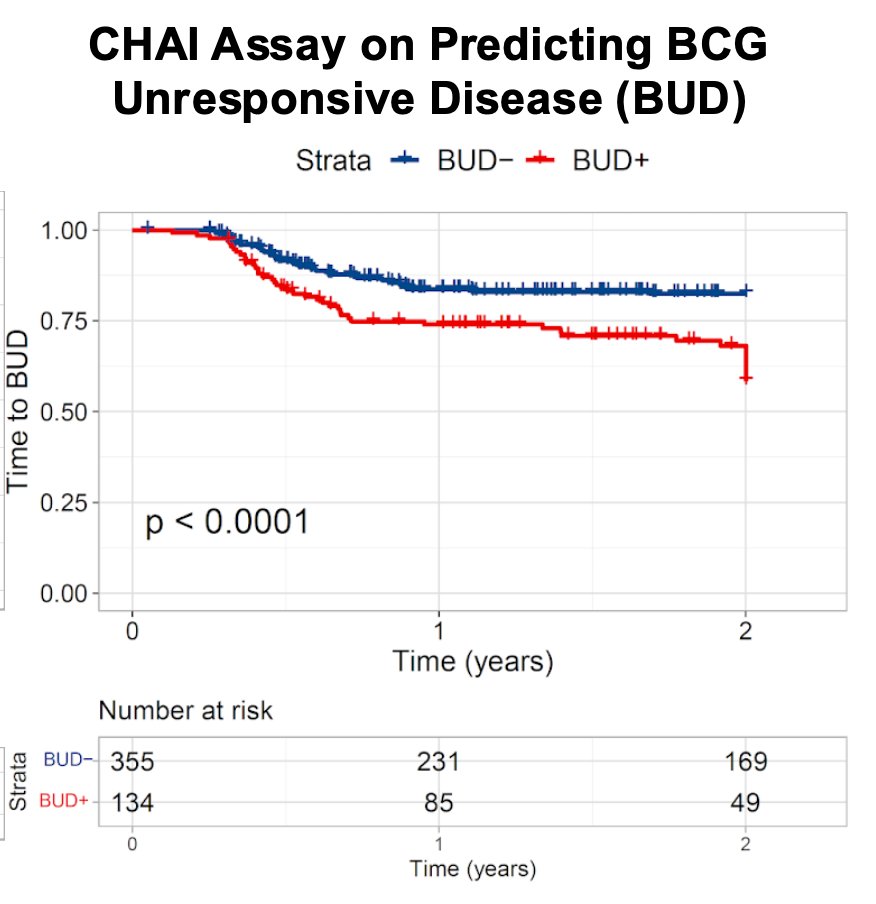
Dr. Packiam concluded his presentation discussing validation of an artificial intelligence-powered pathology assay and comparison to the EAU 2021 guidelines on prediction of muscle-invasive progression post-BCG in an international 12-center cohort by summarizing that this artificial intelligence-powered histologic biomarker utilizing only routine digital histopathology images can identify cases of high-risk NMBIC that are at significantly high risk of recurrence and BCG unresponsiveness.
Presented by: Vignesh Packiam, MD, Rutgers Cancer Institute of New Jersey, New Brunswick, NJ
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, WellStar MCG Health, @zklaassen_md on Twitter during the 2024 International Bladder Cancer Network (IBCN) Annual Meeting, Bern, Switzerland, Thurs, Sept 19 – Sat, Sept 21, 2024


