In the past, cytoreductive nephrectomy was a mainstay of treatment of patients with advanced renal cell carcinoma (RCC). With the publication of CARMENA, upfront cytoreductive nephrectomy has been used less frequently with systemic therapy forming the backbone of first-line treatment. However, there remains uncertainty around managing patients who experience complete or partial responses after systemic therapy and then undergo consolidative nephrectomy.
To better inform the care of these patients, the authors performed a single-institution retrospective study of patients treated with immunotherapy with metastatic cancer at the time of treatment at Memorial Sloan Kettering Cancer Center, including a total of 23 patients. Patients were stratified based on final surgical pathology given the presence of residual disease or pT0. The authors used the Kaplan-Meier method to assess overall survival (OS).
All included patients had metastatic disease at presentation and nearly all had clear cell histology (n=22). Among those patients who had pT0 at time of surgery were treated with combination ipilimumab + nivolumab, were on systemic therapy for almost a year prior to surgery, and had a significant change in size of primary tumor (-3.75cm) prior to surgery. Among the 23 total included patient, 14 (60.87%) had stable metastases or were NED after surgery.
Over a median follow-up of 33 months after surgery, the median overall survival was not reached, however, survival was 52% for patients with residual tumor and 100% for pT0 patients.
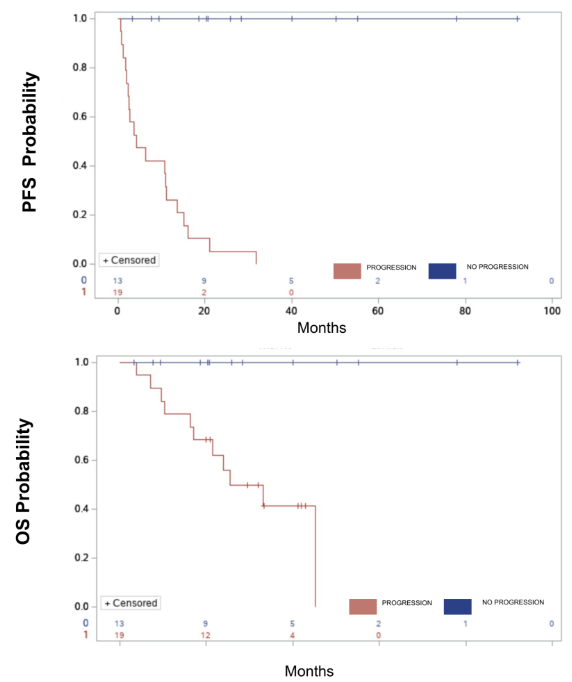
The authors concluded that patients with metastatic disease who demonstrated partial or complete response after immunotherapy and subsequently underwent consolidative nephrectomy had durable overall survival at follow-up, including a sub-set of pT0 patients who were all alive at follow-up.
Presented by: Stephen Reese, MD, MultiCare Rockwood Surgical Specialists, Spokane, WA


