(UroToday.com) The 2022 IKCS North American annual meeting featured a session on multidisciplinary team approaches to rare subtypes, including a presentation by Dr. Kyle Blum discussing biomarkers of disease burden and treatment response in renal medullary carcinoma. Renal medullary carcinoma afflicts young men and women of African descent with sickle hemoglobinopathies. More than 90% have advanced disease and carry an objective response rate of 29% to renal cell carcinoma therapies, with a 13-month median survival. As such, there is a need to develop new ways to screen, diagnose, and treat renal medullary carcinoma to raise its survival curve. Dr. Blum and colleagues established a large renal medullary carcinoma cohort. They assessed known serum tumor markers with renal medullary carcinoma disease severity (e.g. metastatic burden) and correlated marker levels to therapeutic response.
For this study, serum markers were captured in primary renal medullary carcinoma patients treated at MD Anderson Cancer Center within the past 10 years. Those without serum markers were excluded. Inclusion criteria required renal medullary carcinoma diagnosis by either from biopsy or nephrectomy. Using serum tests, known biomarkers in other malignancies were assessed. These markers included CA-125, B2-microglobulin, CEA, AFP, CA19.9, CA15.3, bHCG, and LDH and trended over time with respect to key clinical events including treatment responses, relapses, and progression of disease.
There were 33 patients met criteria, with a median age of 35 years (IQR 22-39), with 70% male, 97% Black, and 97% carrying hemoglobinopathy (e.g. sickle-cell trait or sickle B thalassemia). Overall, 94% presented metastatic at diagnosis. Among these metastatic patients, CA-125 was consistently 20-100x above normal:
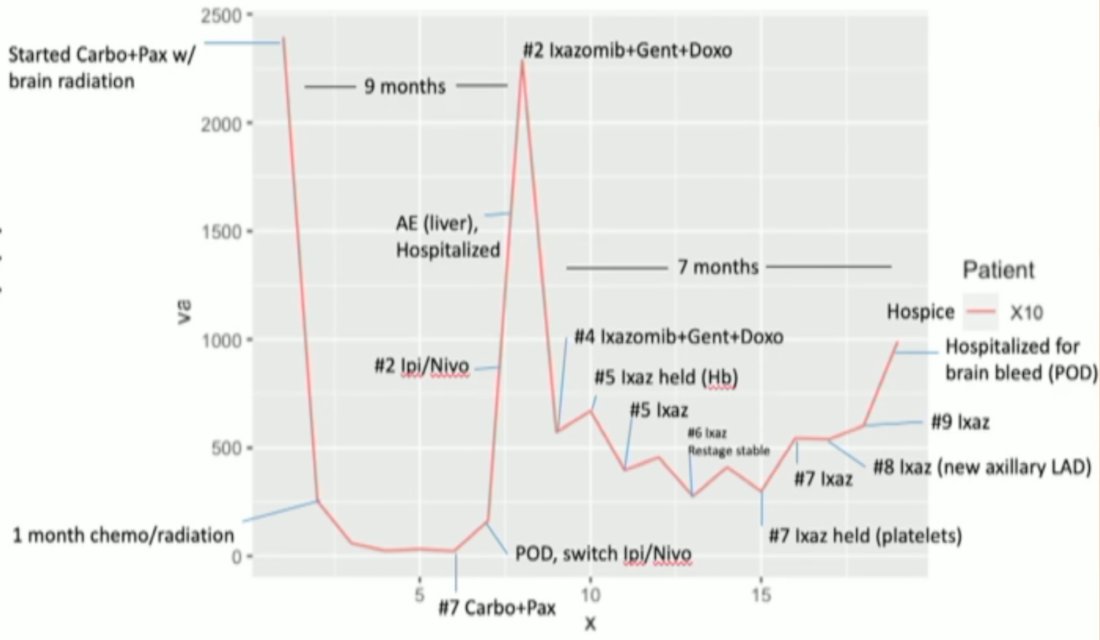
Specifically, 82% of patients had an elevated CA-125 at any point during their disease course and 58% were above the 100 ng/mL threshold. Positive treatment-response resulted in less circulating CA-125 which could be measured over time:
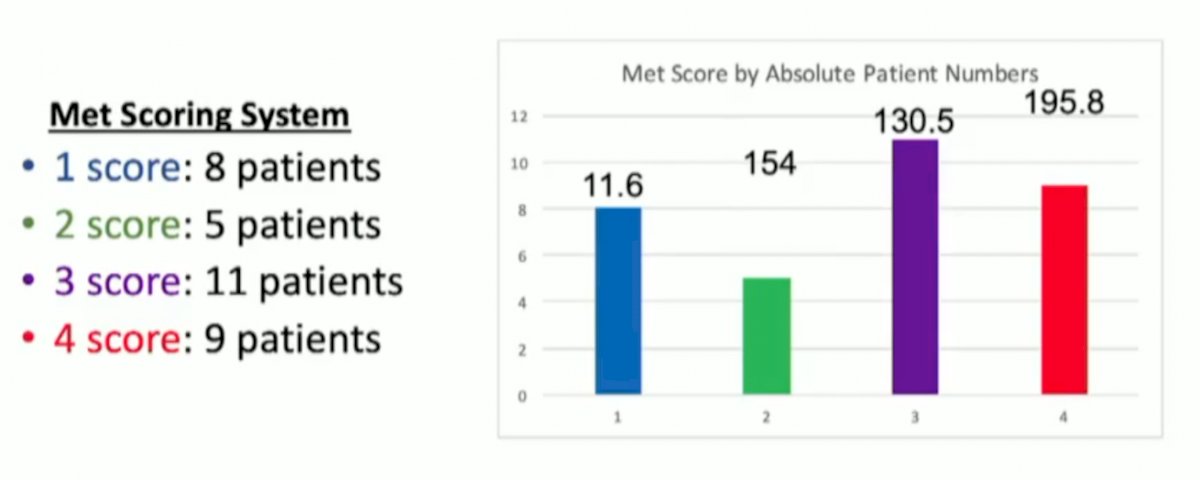
LDH and CA-125 were consistently elevated above upper-limit normal ranges, unlike AFP, CA19.9, CA15.3, and CEA. The magnitude of LDH and CA-125 elevation was directly proportional to metastatic burden with CA-125 levels in widely metastatic patients 200+% higher than upper-limit normal. As follows is the Mets Scoring System highlighted by Dr. Blum:
Dr. Blum concluded his presentation discussing biomarkers of disease burden and treatment response in renal medullary carcinoma with the following take home messages:
- CA-125 correlated with treatment and disease progression
- Increases with worsening disease or metastatic burden
- Decreases with treatment response and decreased metastatic disease
- Implications for moving forward
- Potential marker of disease response and metastatic burden
- Potential therapeutic target
- Reproducible and easily accessible clinically
Presented by: Kyle A. Blum, MD, University of Texas Houston, MD Anderson Cancer Center, Houston, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2022 International Kidney Cancer Symposium (IKCS) North America, November 4-5, Austin, Texas, USA


