(UroToday.com) The tenth session of the 2022 International Kidney Cancer Symposium (IKCS): North America meeting focused on risk stratification in renal cell carcinoma (RCC). In this context, Dr. Hakimi presented on evolving concepts of risk stratification in metastatic RCC.
He began by discussing the MSKCC / Motzer criteria developed in the cytokine era. This was initially developed in the first-line context among patients receiving interferon or interleukin. The five factors in this model, Karnofsky performance status, time from diagnosis, hemoglobin, LDH, and corrected serum calcium, provide useful stratification in terms of patient prognosis: those with favourable disease (no risk factors; 30 months median overall survival), intermediate risk disease (1-2 factors; 14 months OS), and poor risk (3 or more factors; 5 months OS). While developed in this setting, a subset of Motzer criteria (Karnofsky performance status, hemoglobin, and corrected serum calcium) further demonstrated prognostic utility in the second line setting, for example as shown in the context of nivolumab monotherapy in CheckMate025.
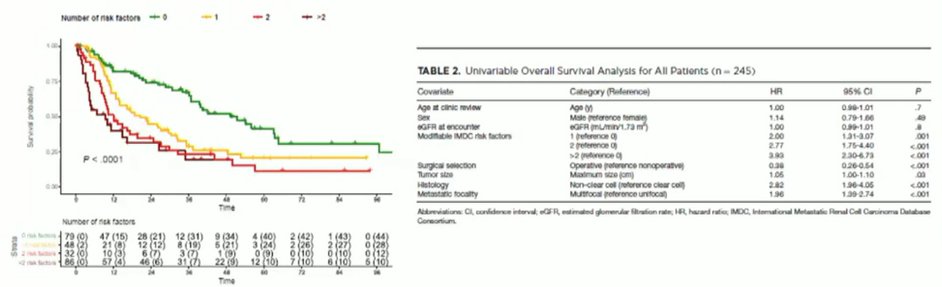
Dr. Hakimi noted that, in modern practice, IMDC / Heng criteria are more commonly used than MSKCC criteria. The Heng criteria include six characteristics, Karnofsky performance status, time from diagnosis, hemoglobin, neutrophil count, platelet count, and corrected serum calcium. These criteria provide very clinically useful prognostication.

In the context of current guidelines, Dr. Hakimi noted that the ASCO guidelines emphasize the importance of risk stratification on the basis of IMDC risk groups in terms of determining first-line systemic therapy as well as the role of cytoreduction. With respect to this second question, Dr. Hakimi noted that observational studies in the immunotherapy era have demonstrated significant benefit to cytoreduction. Importantly, while premised on observational data, he noted that IMDC risk score is significantly prognostic among those patients undergoing cytoreductive nephrectomy.
While IMDC risk score is typically computed at the time of diagnosis of metastatic disease, he noted that is may be dynamic and may change over time, including as a result of therapy. Thus, he emphasized the importance of reassessing risk stratification for patients with mRCC as they undergo treatment. Highlighting work from Dr. Harshman and colleagues, he noted that there may be meaningful rates of reclassification of patients and this may be informative in terms of conditional survival probabilities.
While IMDC risk criteria provide a clinically actionable risk stratification approach, there is always interest in improving our prognostication. Thus, there have been efforts to integrate clinical features with genomic characteristics. As highlighted in work from Voss and colleagues, the addition of genetic information can provide additional prognostic information.

He further noted that there is overlap between what the clinical characteristics used in IMDC risk stratification and genetic characteristics capture.

In closing, Dr. Hakimi noted that risk stratification, across diseases but particularly in mRCC, should be recognized as an ongoing, dynamic process. The clinical risk criteria used today capture an immunosuppressive tumor microenvironment (myeloid high and angio low) for which direct testing may allow refinement of risk stratification approaches. Moving forward, there is an ongoing need and opportunities to reassess risk stratification in the immune checkpoint blockade era.
Presented by: A. Ari Hakimi, MD; Memorial Sloan Kettering Cancer Center


