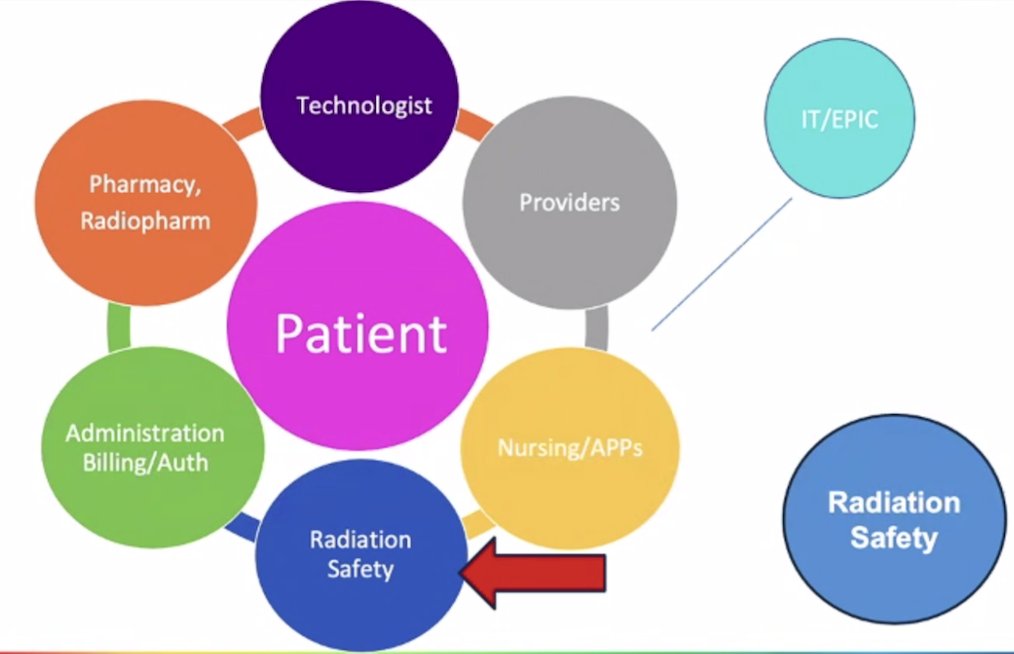
(UroToday.com) The 2024 PSMA conference featured a presentation by Linda Gardner and Amanda Morley (both registered nurses leading their radioligand therapy programs) discussing workflow considerations from the front desk to nursing, including supportive care. Ms. Gardner started by discussing constructing a solid foundation for a radioligand therapy center. This includes going through the appropriate licensing process, deciding where the infusions are going to take place (in IR, oncology, or a shared clinic space), where the restroom and workflow are going to take place, the equipment needed, having a staff and radiation safety plan, deciding hours of operation, and how to handle increasing patient volume and escalations in care. There are several key stakeholders in this program, but it is important to remember that the patient is the most important stakeholder:
Ms. Gardner then discussed obtaining a radioactive materials license. This includes either getting a license from the state or from the Nuclear Regulatory Commission (NRC) (in situations where there is no state governing body) to cover the use of LuPSMA. At UCLA, their license is a Broad Scope Type A license and LuPSMA is covered under “any isotope Z value 3-83”, “any” form. Other types of licenses may need to request an amendment with an agreement state or NRC office in order to add an isotope. This should be taken care of by the Radiation Safety Office, and should be planned ahead given that amendments may take months.
Educating the radioligand therapy team is of the utmost importance. This includes staff training and education, delineating designated roles, and keeping occupational and public doses as low as reasonably acceptable (ALARA). Specific to isotope 177Lu, the half-life is 6.73 days, Beta 498 keV, and Gamma 200 keV. There should be adequate PPE, room prep, take down procedures, and deconstruction in order to minimize contamination and allow appropriate patient release criteria. Equipment training should include real time dosimeter training as well as other specialized equipment in the treatment suite. Real time dosimeters allow real time readings of an individual’s radioactivity exposure:

With regards to actual versus perceived exposure to the staff, the dose to staff (ie. nursing) has been minimal, with approximately <2 mR per procedure (Lu-177 Dotatate from their neuroendocrine program), with an average procedure for Lu-177 Dotatate taking ~5-6.5 hours.
Shifting to administration, billing, and authorization, Ms. Gardner emphasizes that there are important stakeholders here as well. It is important to understand the authorization process, the logistics of scheduling multiple visits, billing/pricing/coding, and instituting a dynamic schedule in case there are cancellations. Programs should have access and training for online ordering, have backup plans in place, and track everything with an Excel spreadsheet. For IT and EPIC, there should be a therapy plan for all cycles, built in order sets in order to align treatment and ordering for all treating departments, and automated discharge information. The electronic workflow should be incorporated, including the consent process and ID arm band scanning.
At UCLA, there radiopharmacy uses the ROME online ordering system, which includes batch releases, and point of contact in cases there are delays or cancellations. It is important to have specific delivery days for the clinic, understand the hours of delivery, and to have a hot lab that receives the doses.
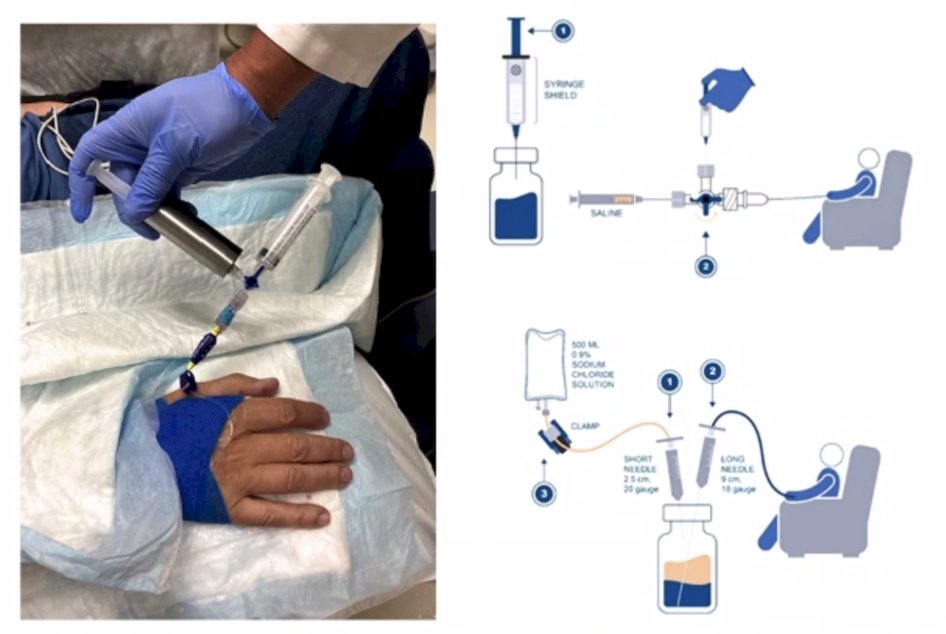
The nuclear medicine technologists are an integral part of formulating standard operating procedures, receiving and inspecting doses, performing calibration, and preparing doses. Additionally, technologists are important for ensuring patient safety and monitoring safety practices. There are several infusion options for LuPSMA, as highlighted in the following figure (left: slow IV hand injection method):
On the day of the patient’s infusion, there are several important points of consideration:
- Managing patient expectations
- Orienting the patient
- Review of the treatment process
- Obtaining consent from the patient by the treating physician
- IV hydration prior to therapy
- Ensuring the patient has spare clothing
- Having a dedicated registered nurse
- Addressing any patient concerns
Once IV hydration is complete, with the physician present, the dose is verified next to the patient, radiation precautions are in effect, and the IV site is checked. The treatment is then administered by the slow IV hand injection method, the IV is flushed with normal saline, and the treatment is complete. At the time of discharge, the patient is given their discharge instructions, a wallet card, and is schedule for follow-up. They are also provided with contact information, scripts (if needed), they void in the rest room, and are discharged with a dosimetry read of 1 meter. The new treatment space at UCLA (about to open) is below:

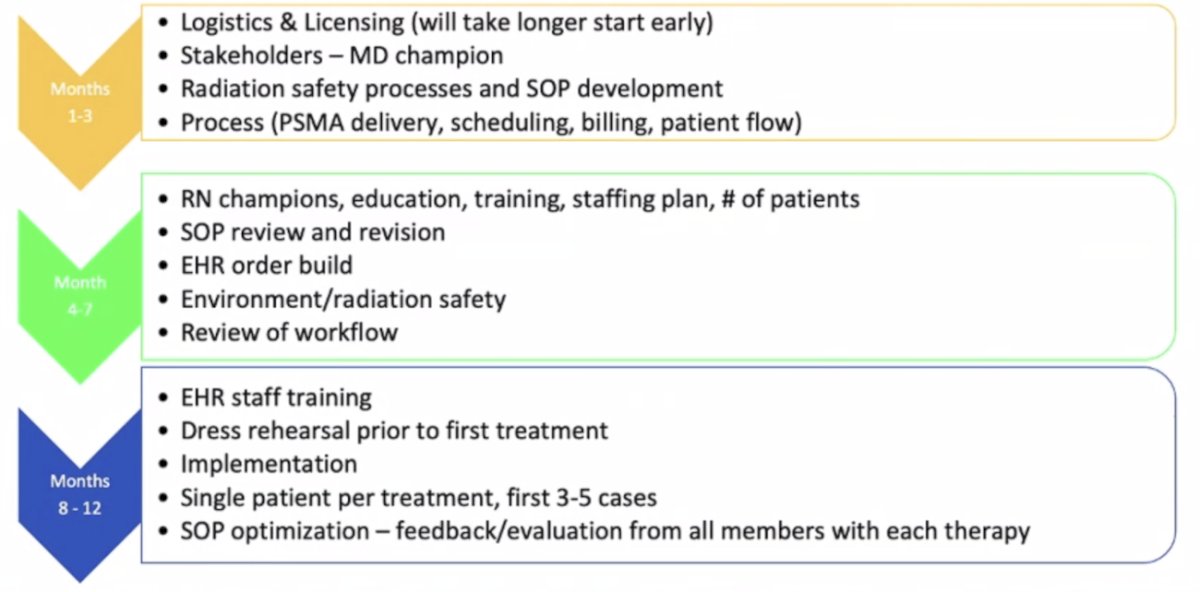
According to Ms. Gardner, the ideal PSMA Program Development Timeline occurs over 8-12 months, as follows:
Ms. Morley then discussed their experience at UCSF, which is centered around shared resources, including the treatment space, SPECT/CT scanner, clinical nurses, and nuclear medicine technologists. Their treatment space is currently as follows:

Ms. Morley emphasized that their work flow includes the referral consultation insurance status patient education treatment. Their radioligand therapy team includes physicians, nurse practitioners, practice coordinators, and registered nurses. Perhaps unique, all of their patients receiving LuPSMA have a nuclear medicine physician, as well as a GU medical oncologist on the treatment team. According to Ms. Morley, making sure the referral is done and checked appropriately is very important. This includes:
- Checking the requirements for the referral
- Assessing whether the patient meets criteria for treatment
- Assessing pre-chemotherapy patients
- Assessing if the patient is an appropriate patient for this type of outpatient treatment (ie. appropriate ECOG status, how far are they travelling from, family/friend support, etc)
The initial consultation for these patients is 60 minutes, where potential side effects are discussed, a long discussion is held regarding radiation safety, patient education commences, patient expectations are addressed, and the therapy plan is formulated. Since appropriately ordered LuPSMA is a standard of care, typically insurance nuances are delineated by whether the patient has Medicare versus commercial insurance. After initial patient education in the first consultation, this education continues with the nursing staff, the nurse navigator having a planning call with the patient, consent being obtained on the day of treatment by the physician, written instructions, and follow-up phone calls and visits. When discussing radiation safety with the patient, this includes risk of contamination from incontinence, specific discharge instruction in the first 72 hours after treatment, stressing the importance of distancing from others (in particular, pregnant women and children), increasing fluid intake, and proper urinary waste. Common side effects are discussed with the patient, including bone marrow toxicity.
The treatment workflow for LuPSMA patients is typically treatment 6 weeks apart and up to 6 cycles of therapy. These patients undergo a post-infusion SPECT/CT, have labs drawn mid-cycle, have CT scans after every 2 cycles, and have follow-up visits four weeks after infusion. GU medical oncology follow-up is after the six cycles are complete.
Linda Gardner and Amanda Morley concluded their presentation discussing workflow considerations from the front desk to nursing, including supportive care with the following lessons learned and recommendations:
- It is important to have early involvement of stakeholders
- Staff should be involved early, including education (no assumptions should be made and it is important to identify knowledge gaps)
- There should be continuous communication
- The team should adapt to their environment
- Expect deviations from the plan
- Care coordinators/nurse navigators are crucial
Presented by: Linda Gardner, UCLA, Los Angeles, CA, Amanda Morley, UCSF, San Francisco, CA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 PSMA Conference, San Francisco, CA, Thurs, Jan 18 – Fri, Jan 19, 2024.
Related content: Workflow Considerations from the Front Desk to Nursing Including the Supportive Care Idea: The UCLA/UCSF Experience "Presentation" - Linda Gardner & Amanda Morley
View: Video Series on
Integrating (177Lu)–PSMA-617: A Practical Approach for Urology Clinics
Practical Aspects of Operationalizing Lutetium-177 (177Lu)–PSMA-617 in the Urology Clinic


