(UroToday.com) One of the main hot topics of the entire Retreat discussed by different speakers pinpoint the relevant advances and main changing in the imaging in GU oncology. Prof Alberto Briganti opened the first talk of the Meeting speaking about Prostate Cancer, and during the first part of the presentation he spoke about the “imaging revolution”. “We assisted in the last 10 years at an imaging revolution. In 2014 MRI was suggested in EAU guidelines for patients with an initial negative biopsy and candidates to repeat prostate biopsy. Now, according to the last version of EAU guidelines1 with a strong level of evidence MRI is recommended in every patient with elevated PSA and suspicion of prostate cancer. “Introducing MRI in our diagnostic processes we assisted to a decrease in unnecessary prostatic biopsies.“
MRI has a high negative predictive value, but an “extremely low positive predictive value” of 40%2 “There are grey zones, and the grey zones of MRI are huge” due to high inter-reader variability, hence “ the expertise of the radiologist is key to give MRI indication for biopsy” said Prof. Briganti. Another issue related to the overgrading of what is inside the sample, and undegrading what is outside the sample. A possible solution suggested was to use regional targeted biopsies, but still, according to the “provocative statistical analyses” led by Dr. Vickers,3 even in the best statistical scenario possible we needed to diagnose 89 Prostate cancer (PCa) to prevent 1 PCa death.
Another hot topic discussed regarding the imaging revolution in the GU oncology field was the usage of PET-CT scans. During the keynote lecture on “the role of PET imaging in GU cancer “Prof. Fanti showed the settings in which PET CT can provide additional information, showing the little played by FDG-PET/CT and the paucity of data published on nodes evaluation in UTUC, or on the evaluation of residual disease in testicular cancer but “it is in the setting of PCa where PET-CT plays its biggest role” said Prof. Fanti. Through an interesting chronological picture Prof, Fanti showed the evolution of technics and indications of Nuclear medicine methodologies, provocatively comparing the low image resolution of Bone scans to “stone age cave paintings” and the low sensitivity of PET-coline to “ impressionism painting”. Talking about PSMA PET/CT prof. Fanti defined it as a “revolution”, with higher sensitivity compared to PET-coline and conventional imaging4 [CT and bone scan], but no data about OS improvement on its usage. In a recent consensus meeting, 77% of the expert involved in a panel consultation voted to recommend PSMA-PET in high-risk disease as a staging examination” however, to date no outcome data exist to inform subsequent management. “The real question is how to deal with lesions diagnosed only on a PSMA PET but not on conventional imaging when all the available studies are based on conventional imaging, and also considering that PSMA PET does have false positives”, said Prof. Briganti. “All the evidence of Metastases Direct Therapy (MDT) are based on three phase 2 study with no more than 150 patients, these studies have shown that it may decrease the initiation of ADT and increase the rate of cancer control early after therapy, but no data about the long term. We are changing our attitude based on hundred patients randomized in 3 phase 2 trials, and “we need to be very careful” said Briganti.
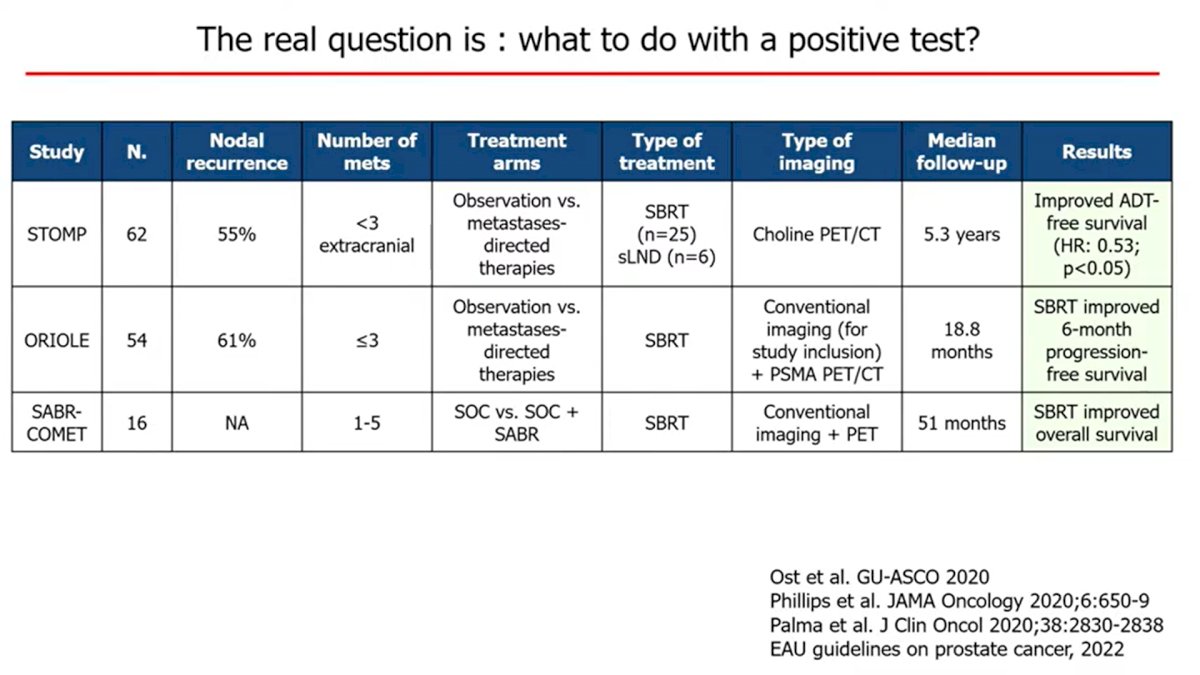
According to an expert panelist consensus [APCCC 2022], for metachronous mHSPC low volume on next generation Imaging and nonmetastatic on conventional imaging 82% of the experts voted for MDT alone or in combination with systemic therapy.
Prof. Fanti underlined that due to a spatial resolution of 3-4 mm, micrometastases will be always missed, moreover, he pinpoint that a negative PSMA-PET/CT in high-risk patients cannot allow for avoiding lymphadenectomy. Also prof. Briganti during his talk spoke about the nonmetastatic CRPC (nmCRPC), defining the m0CRPCP setting as “just a possible artificial setting” only related to the not sufficient enough imaging sensitivity.
Speaking of the biochemical recurrent setting, defined by Prof. Fanti as “the bread and butter and main indication of PSMA-PET/CT in PCa”, according to EAU guidelines either after radical prostatectomy or radiotherapy PSMA PET is strongly recommended (2b level of evidence)i. PSMA-PET/CT was shown to have a higher detection rate in early recurrence compared to other imaging modalities, especially in patients with low PSA.5 In a study by Fendler et al, 200 men previously diagnosed with high-risk m0CRPC, 98% (196/200) resulted positive to PSMA PET,6 “it is even questionable if m0CRPC even exists, it is only about what strategy you use to study the patient” said Prof. Fanti.

Presented by:
- Alberto Briganti, MD,Ph.D. Urology San Raffaele University Hospital, Milan, Italy
- Fanti Full, Professor, S. Orsola University Hospital, Bologna, Italy
- Giorgio Brembilla MD, Ph.D, Radiology, San Raffaele University Hospital, Milan, Italy
References:
- “EAU Guidelines on Prostate Cancer.” Uroweb. Accessed 2022. https://uroweb.org/education-events/eau-guidelines-on-prostate-cancer.
- Mazzone et al., Risk Stratification of Patients Candidate to Radical Prostatectomy Based on Clinical and Multiparametric Magnetic Resonance Imaging Parameters. European urology. 2021. 81(2):193-203.
- Andrew J. Vickers. Effects of Magnetic Resonance Imaging Targeting on Overdiagnosis and Overtreatment of Prostate Cancer. Eur Urol 2021;80:567–72
- Hofman et al., Prostate-Specific Membrane Antigen PET-CT in Patients with High-Risk Prostate Cancer before Curative-Intent Surgery or Radiotherapy (ProPSMA). Lancet. 2020 Apr 11;395(10231):1208-1216.
- De Visschere et al., A Systematic Review on the Role of Imaging in Early Recurrent Prostate Cancer. Eur Urol Oncol. 2019 Feb;2(1):47-76.
- Fendler et al., Prostate-Specific Membrane Antigen Ligand Positron Emission Tomography in Men with Nonmetastatic Castration-Resistant Prostate Cancer. Clin Cancer Res. 2019 Dec 15;25(24):7448-7454.


