(UroToday.com) The 2024 Southeastern Section of the AUA (SESAUA) annual meeting featured a Health Services Research and Socioeconomics session and a presentation by Avani Desai discussing the feasibility and outcomes of interventions to reduce cystoscopy discomfort. Each year, over a million individuals undergo office cystoscopy for bladder cancer diagnosis and surveillance.1
Approximately one-third of patients experience major discomfort during office cystoscopy, and over 40% of bladder cancer patients have substantial anxiety associated with cystoscopy.2 Thus, reducing cystoscopy discomfort is among the highest areas of importance for bladder cancer patients and their caregivers.3 A previously published meta-analysis evaluated studies for reducing this discomfort through medical or environmental methods, with these interventions having evidence of efficacy, but not yet being widely implemented or compared with each other.4 As such, Avani Desai and colleagues initiated a quality improvement project that explored interventions to decrease pain and anxiety among cystoscopy patients. The objectives of this study were to assess efficacy of interventions to decrease pain and anxiety during cystoscopy and to understand implementation challenges to inform design of a future comparative effectiveness trial.
In this study, 110 adults underwent office cystoscopy at the University of North Carolina. Participants were offered 20 mL intraurethral 2% lidocaine with a dwell time of ≤10 or >10 minutes and either listening to music on headphones or real-time visualization of cystoscopy:
If a patient declined the offered intervention, their requested intervention was provided and recorded. After the procedure, patients recorded pain during cystoscopy on the Visual Analog Scale (VAS; range 0-10), pain intensity (PROMIS; range 1-5), and emotional distress-anxiety.
The majority of patients received cystoscopy for bladder cancer surveillance (57.3%) or hematuria evaluation (26.4%), with patients averaging 3.91 prior cystoscopies (SD 6.16). Each intervention was offered to 23-27% of patients:
Overall, 30 patients declined their offered inventions, 25 of whom were offered music and instead requested visualization: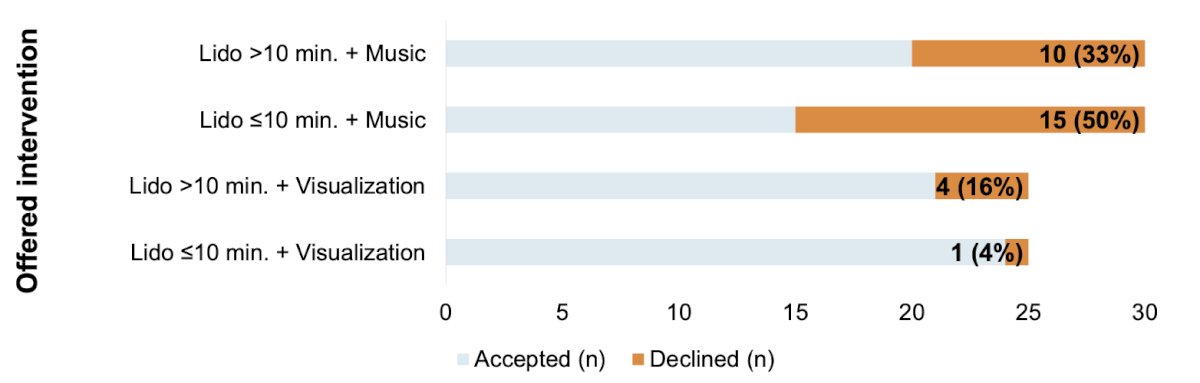
Most declining patients presented for bladder cancer surveillance (67%) or hematuria (20%) and had undergone cystoscopy previously (73%). Multiple regression analysis controlling for age, number of prior cystoscopies, and cystoscopy indication showed that visualization (t = -3.21, p = 0.002) and music (t = -2.25, p = 0.027) were independently associated with decreased VAS, whereas increased lidocaine dwell time was not (t = -1.62, p = 0.109). Similarly, visualization (t = -3.79, p < 0.001) and music (t = -3.72, p < 0.001) were independently associated with reduced PROMIS Pain, measuring pain intensity, whereas increased lidocaine dwell time was not (t = -0.24, p = 0.813):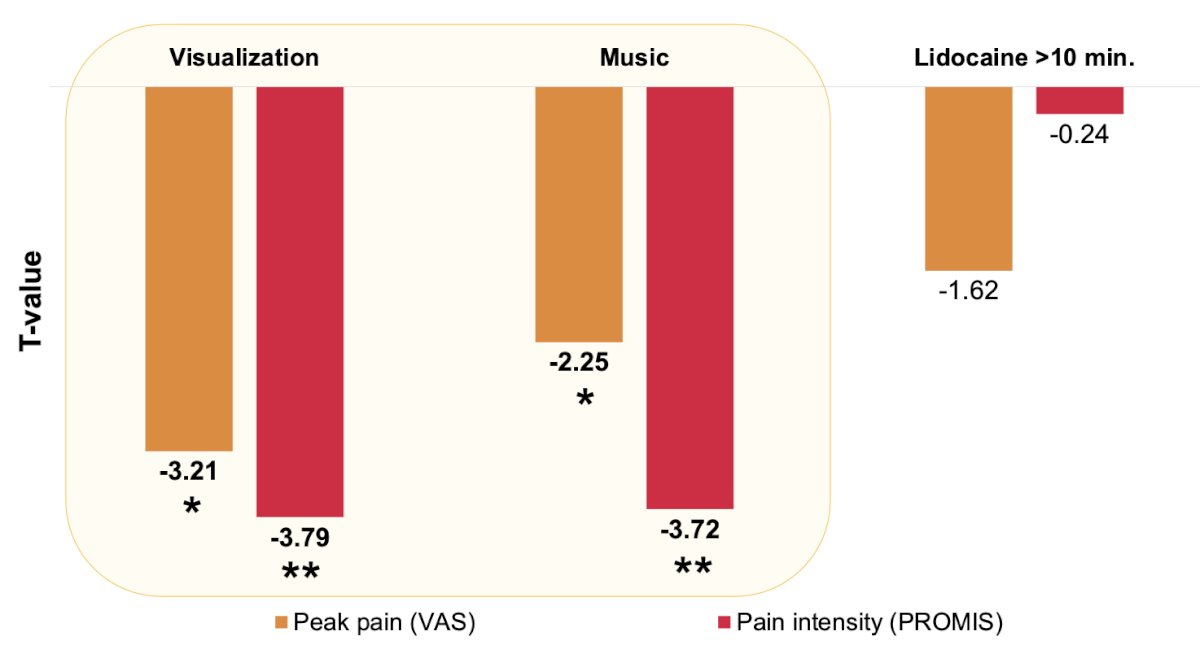
No intervention was significantly associated with reduced emotional distress-anxiety.
Avani Desai concluded her presentation discussing the feasibility and outcomes of interventions to reduce cystoscopy discomfort with the following summary statements:
- Visualizing office cystoscopy in real-time or listen to music during the procedure are simple, accessible, and efficacious means of significantly reducing pain and discomfort related to cystoscopy
- Visualization may be particularly valuable for patients presenting for bladder cancer surveillance, for potential bladder cancer diagnosis, or those who have had a cystoscopy before, as these individuals tended to reject alternate environmental interventions in favor of visualization
- Defining the effectiveness of patient-centered interventions to reduce cystoscopy discomfort can increase tolerance of an invasive procedure, and improve adherence to recommended follow-up cystoscopy procedures
Future directions include evaluation of these interventions in a large, multi-institutional, randomized trial to further compare efficacy and assess which interventions work best for different patient subgroups, allowing for the implementation of more tailored approaches.
Presented by: Avani Desai, MD Candidate, University of North Carolina, Chapel Hill, NC
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Southeastern Section of the American Urological Association (SESAUA) Annual Meeting, Austin, TX, Wed, Mar 20 – Sat, Mar 23, 2024.
References:
- Van der Aa MNM, Steyerberg EF, San EF, et al. Patients’ perceived burden of cystoscopic and urinary surveillance of bladder cancer: A randomized comparison. BJU Int 2008;10(9):1106-1110.
- Kukreja JB, Schroeck FR, Lotan Y, et al. Discomfort and relieving factors among patients with bladder cancer undergoing office-based cystoscopy. Urol Oncol. 2022;40(1):9.e19-9.e27.
- Hamad J, Gore J, Chisolm S, et al. Patient empowerment through engagement in bladder cancer research. Urol Oncol. 2021;39(3):193.e13-193.e19.
- Raskolnikov D, Brown B, Holt SK, et al. Reduction of pain during flexible cystoscopy: A systematic review and meta-analysis. J Urol. 2019;202:1136-1142


