The authors identified and analyzed the number of uncomplicated cystoscopies (CPT 52000) performed between 2009 and 2021 in the MarketScan commercial claims (CCAE) and Medicare supplemental database (MDCR). Cystoscopies associated with any other procedures were excluded from the analysis. Observed counts of procedures were reported per 100,000 eligible enrolled patients in each given year. Costs for CPT code 52000 were inflation-adjusted for the year 2021 for reporting. All comparisons were tested by Chi-square for categorical and Wilcoxon rank-sum test for continuous variables.
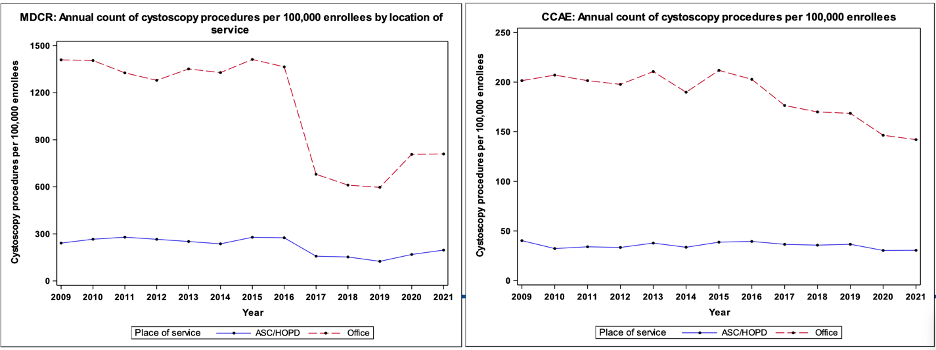
A comparison of the annual count of cystoscopies performed in the office as compared to ASC per 100,000 enrollees in both CCAE and MDCR datasets shows that the number of cystoscopies performed in office has slowly declined over time, whereas the number of procedures in ASCs has remained stable:
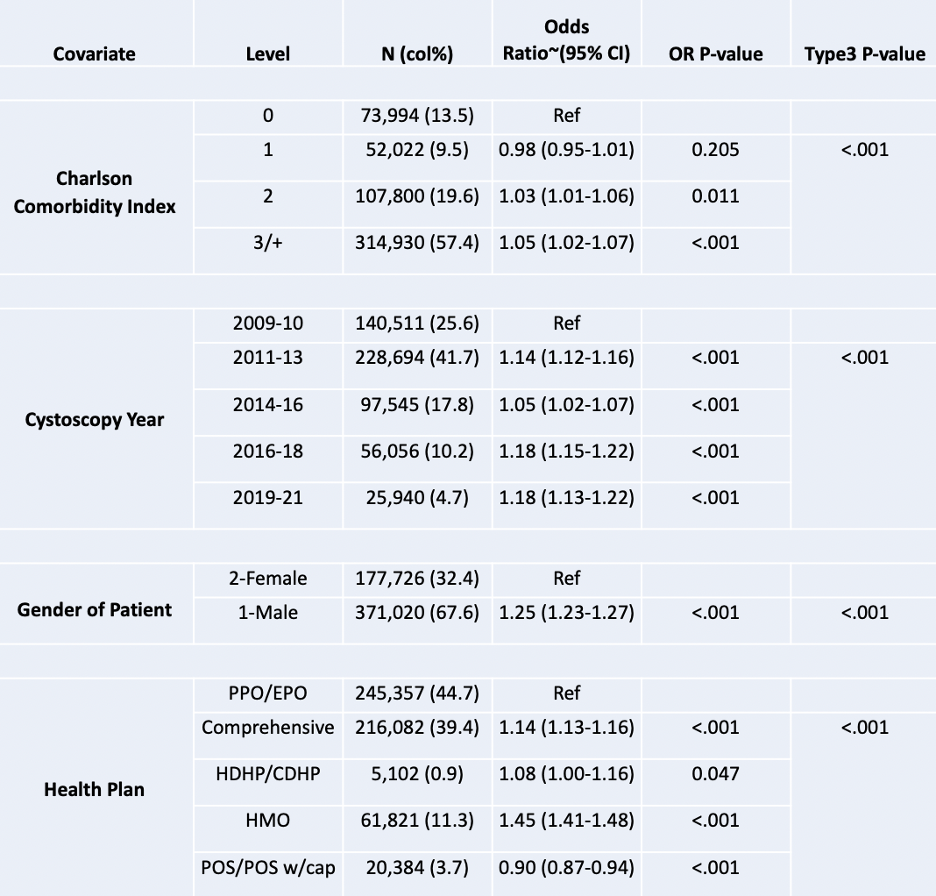
For the MDCR cohort, multivariable logistic model for location of cystoscopy and demographics noted that patients with CCI >= 3 were 5% more likely to have an ASC-based cystoscopy. Additionally, in the years 2019-2021, 18% more cystoscopies were ASC-based compared to 2009-2010, male patients were 25% more likely to have a cystoscopy done in an ASC, and patients with HMO plans were 45% more likely to have an ASC-based cystoscopy compared to patients with PPO plans:
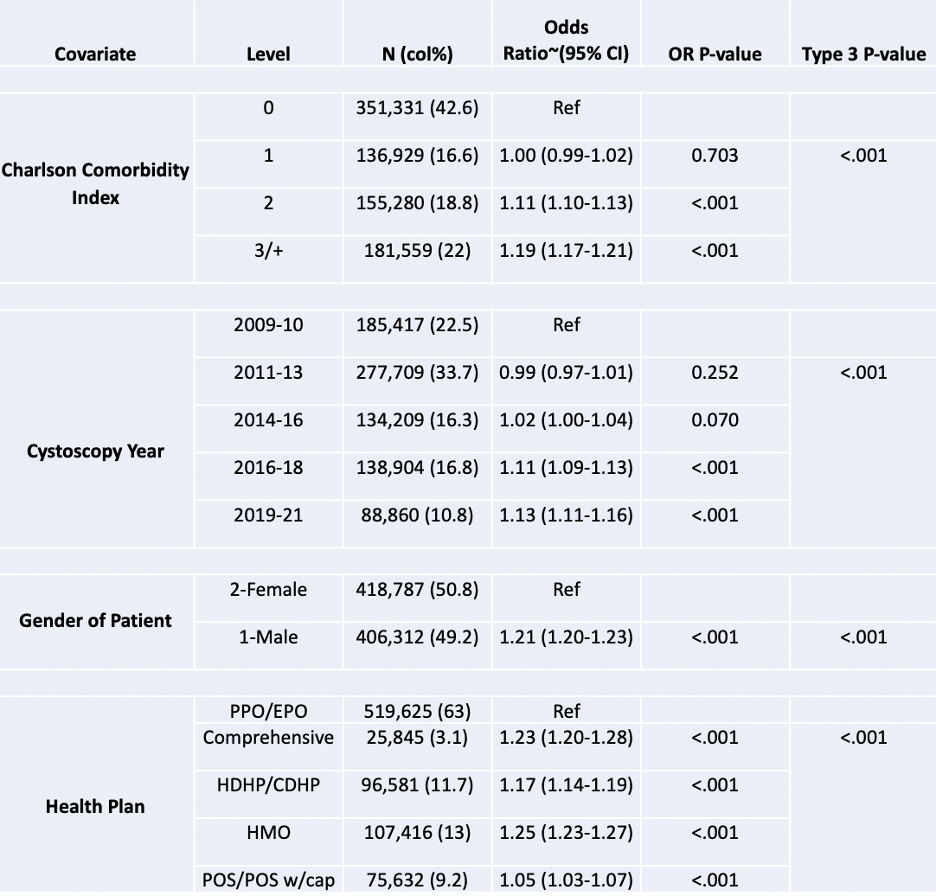
For the CCAE cohort, multivariable logistic model for location of cystoscopy and demographics noted that patients with CCI >= 3 were 19% more likely to have an ASC-based cystoscopy. Additionally, in the years 2019-2021, 13% more cystoscopies were ASC-based compared to 2009-2010, male patients were 21% more likely to have a cystoscopy done in an ASC, and patients with HMO plans were 25% more likely to have an ASC-based cystoscopy compared to patients with PPO plans:
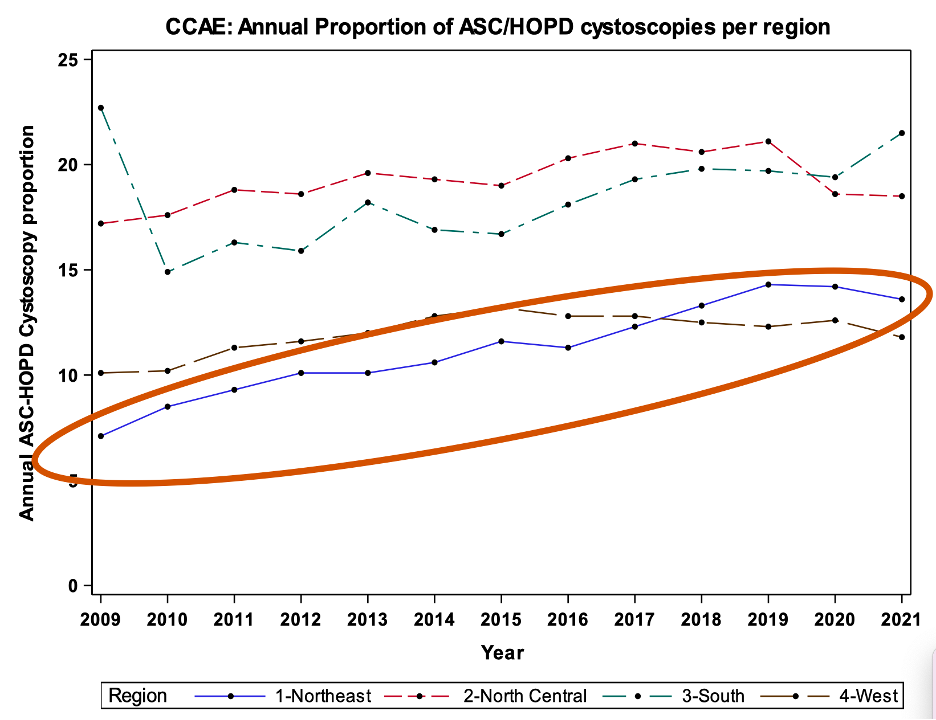
With regards to the proportion of ASC cystoscopies per region for CCAE, there was a statistically significant increase in the proportion of ASC cystoscopies in the Northeast, with a proportionate increase driven by the drop in office-based cystoscopy over time:
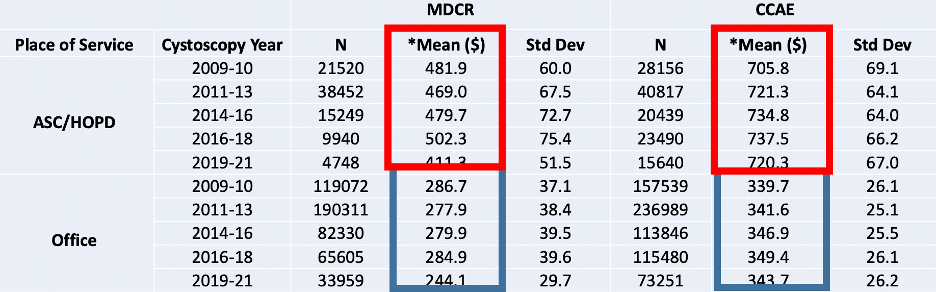
Dr. Joshi also noted that the cost of cystoscopy is always higher when performed in an ASC versus an office setting. As follows is the predicted inflation-adjusted total payments for cystoscopy by location:
Dr. Joshi concluded his presentation by discussing the prevalence, trends, and costs of office-based and ASC-based diagnostic cystoscopy in the United States with the following conclusions:
- The proportion of ASC-based diagnostic cystoscopy has slightly shifted over time
- The number of office-based cystoscopy has overall declined while the number of ASC-based procedures has remained stable over years. Whether this is due to de-escalation of care or advances in non-invasive technology or novel therapeutics over time remains to be elucidated
- There is a significant cost difference between office-based and ASC-based cystoscopy
- The increasing proportion of ASC-based diagnostic cystoscopies over time should prompt further research focusing on appropriate resource utilization for these procedures
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Southeastern Section of the American Urological Association (SESAUA) Annual Meeting, Austin, TX, Wed, Mar 20 – Sat, Mar 23, 2024.


