(UroToday.com) The 2024 Southeastern Section of the AUA (SESAUA) annual meeting featured a kidney cancer session and a presentation by Dr. Sol Moon discussing intravascular heparinization during IVC thrombectomy and perioperative complications. IVC tumor thrombectomy is a complex operation and frequently requires venous cross-clamping for reconstruction. Although the use of subcutaneous prophylactic heparin is standard for the prevention of thromboembolic events, the use of IV heparinization prior to IVC clamping is not. Dr. Moon and colleagues sought to evaluate and compare the characteristics and postoperative outcomes of patients undergoing radical nephrectomy with level I or higher IVC tumor thrombectomy who received IV heparinization versus those who did not. The hypothesis for this study was that for patients undergoing IVC tumor thrombectomy, IV heparinization at the time of IVC cross-clamping is safe and does not contribute to an increased risk of post-operative complications.
This study reviewed patients who underwent radical nephrectomy with IVC tumor thrombectomy between 2015-2023 at the University of Alabama-Birmingham. Patients were grouped by having received or not received IV heparinization intraoperatively. Dr. Moon recorded and compared baseline characteristics intraoperative data and post-operative outcomes. Categorical outcome variables were compared using 2-sided Chi-squared tests, or 2-sided Fisher’s exact test when appropriate. Additionally, an a-priori multivariable logistic regression was performed for significant univariate outcome findings.
Overall, 94 patients underwent nephrectomy with tumor thrombectomy. Seventy-six patients had a level 1 or greater IVC tumor thrombectomy. Among these patients, 30 (39%) received IV heparin and 46 (61%) did not. The complete patient baseline characteristics are as follows:
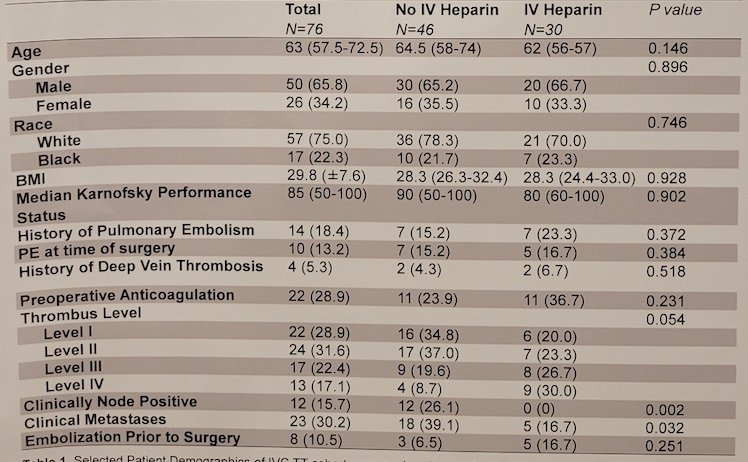
Overall, 67 (88%) required IVC repair, with a mean IVC clamp time of 12 minutes. IV heparin use was associated with higher thrombus level (p = 0.054), stage (p = 0.002), metastatic disease (p = 0.032), longer operative time (362 minutes vs 271.5 minutes, p < 0.001), IVC repair (100% vs 80.4%, p = 0.01) and estimated blood loss (p = 0.075). IV heparin use was not associated with multispecialty surgical teams. Any complication was associated with IV heparin use (p = 0.035), but this was not true when grouped to major or minor complications (p = 0.332). No differences were observed for post-op venous thrombotic events (p = 0.543), post-operative blood transfusions (p = 0.729), and readmission (p = 0.295).:
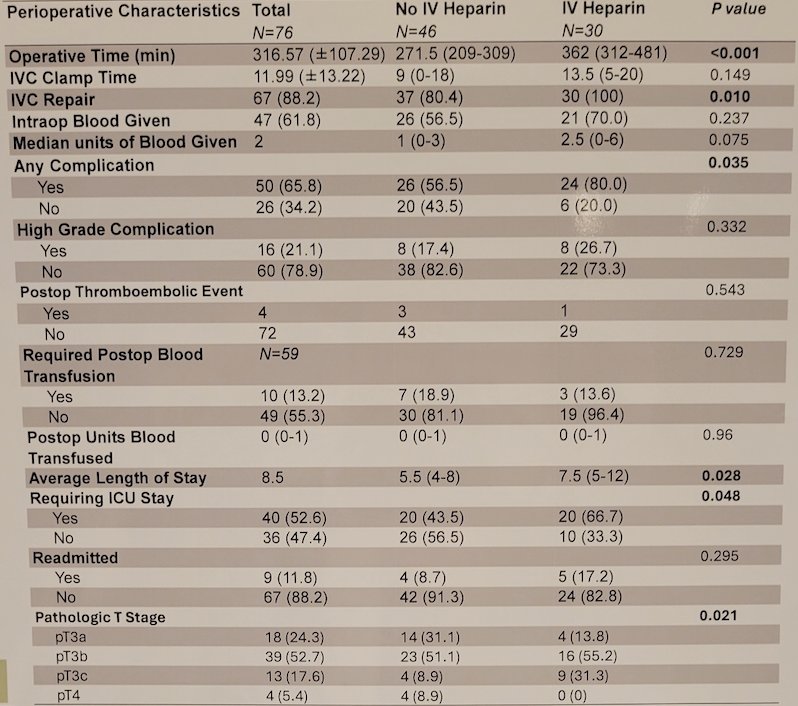
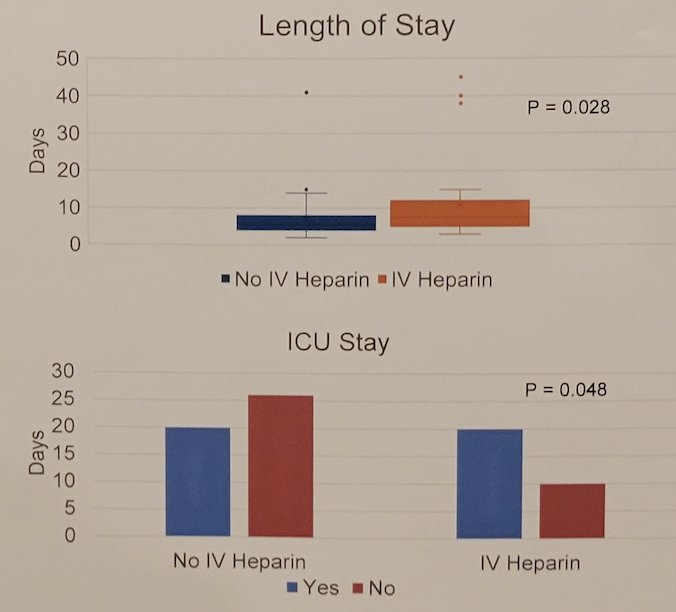
Patients in the IV heparin group were more likely to have a longer length of stay (mean 5.5 vs 7.5 days, p = 0.028) and require ICU level of care (p = 0.048):
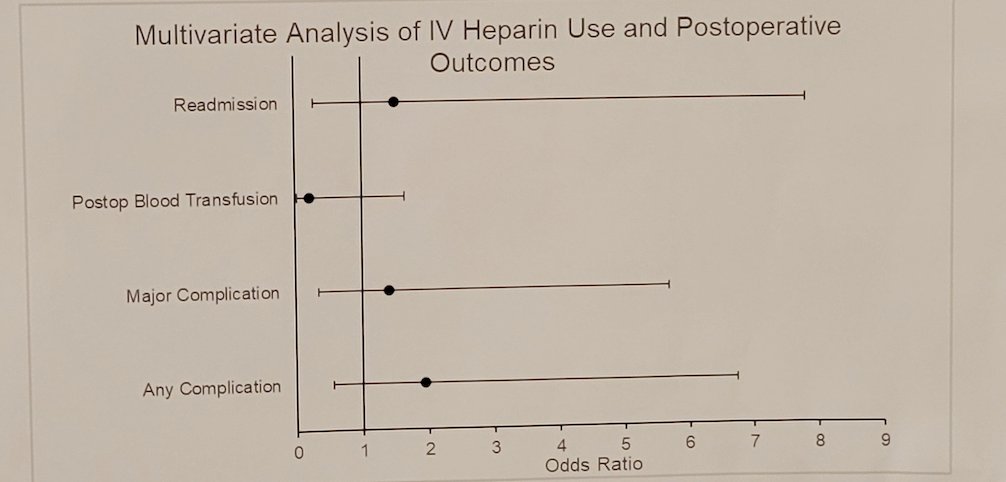
On multivariable analysis adjusting for age, sex, thrombus level, and clinical metastases, IV heparinization was not associated with an increased risk of any complication, major complication, blood transfusion, or readmission:
Dr. Moon concluded his presentation by discussing intravascular heparinization during IVC thrombectomy and perioperative complications with the following conclusions:
- The IV heparin cohort was associated with advanced pathologic stage, longer operative time, requiring IVC repair, increased length of stay, and need for ICU care
- The IV heparin cohort had a significantly increased rate of any complication, however, there was no significant difference in major complication rates between the two cohorts
- The was no difference in postoperative thromboembolic events between either cohort
- An a priori multivariable analysis suggests that there is no increased risk when controlling for multiple patient characteristics, suggesting that use of IV heparin is safe during IVC tumor thrombectomy and can be used at the discretion of the treating surgeon
Presented by: Sol Moon, MD, University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 Southeastern Section of the American Urological Association (SESAUA) Annual Meeting, Austin, TX, Wed, Mar 20 – Sat, Mar 23, 2024.


